CASE20230825_040
A STEMI Patient With Cardiogenic Shock And Heavily Calcified Unprotected Left Main Disease
By You-Ning Chang, Chuan-Tsai Tsai
Presenter
You-Ning Chang
Authors
You-Ning Chang1, Chuan-Tsai Tsai1
Affiliation
Taipei Veterans General Hospital, Taiwan1,
View Study Report
CASE20230825_040
High-Risk Intervention - High-Risk Intervention (Diagetes, Heart Failure, Renal Failure, Shock, etc)
A STEMI Patient With Cardiogenic Shock And Heavily Calcified Unprotected Left Main Disease
You-Ning Chang1, Chuan-Tsai Tsai1
Taipei Veterans General Hospital, Taiwan1,
Clinical Information
Relevant Clinical History and Physical Exam
A 70-year-old woman had DM and RA history, presented with chronic angina pain for a month. She felt hesitated about intervention after Thallium Scan revealed positive results. After two more weeks, she went to our ED room for intolerant chest pain. At triage, vital signs were 35.3 temperature, 140 pulsation and 21 respiratory rate with NIBP 118/69. She felt alert and warm extremities while at ED.
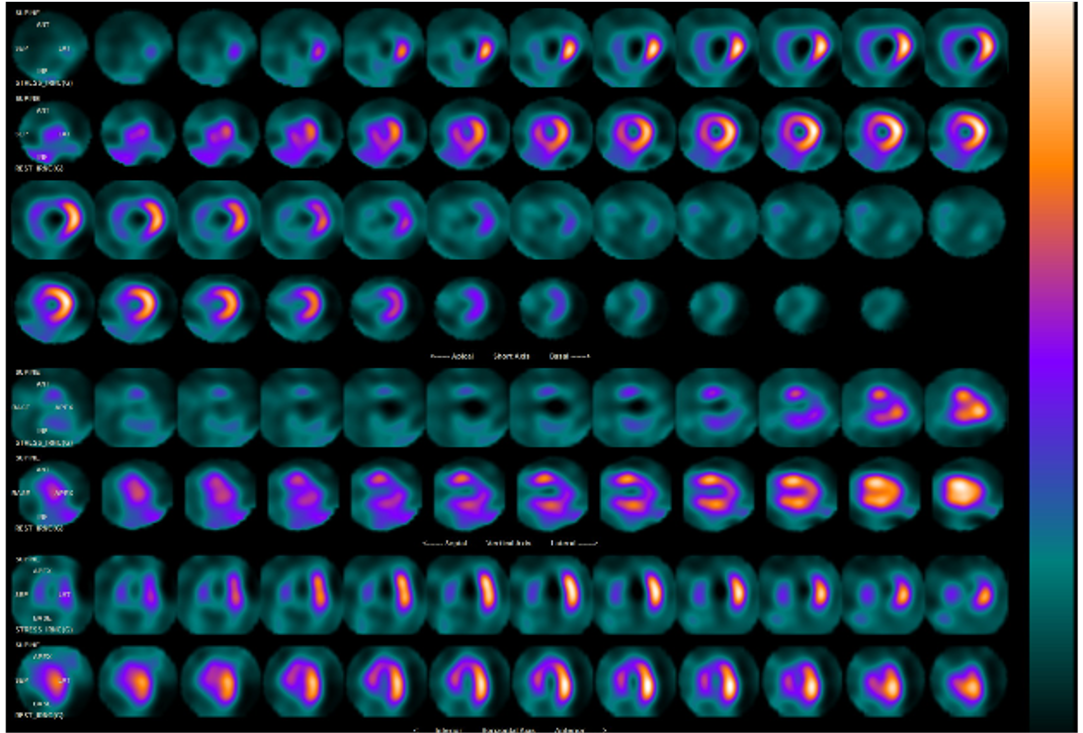
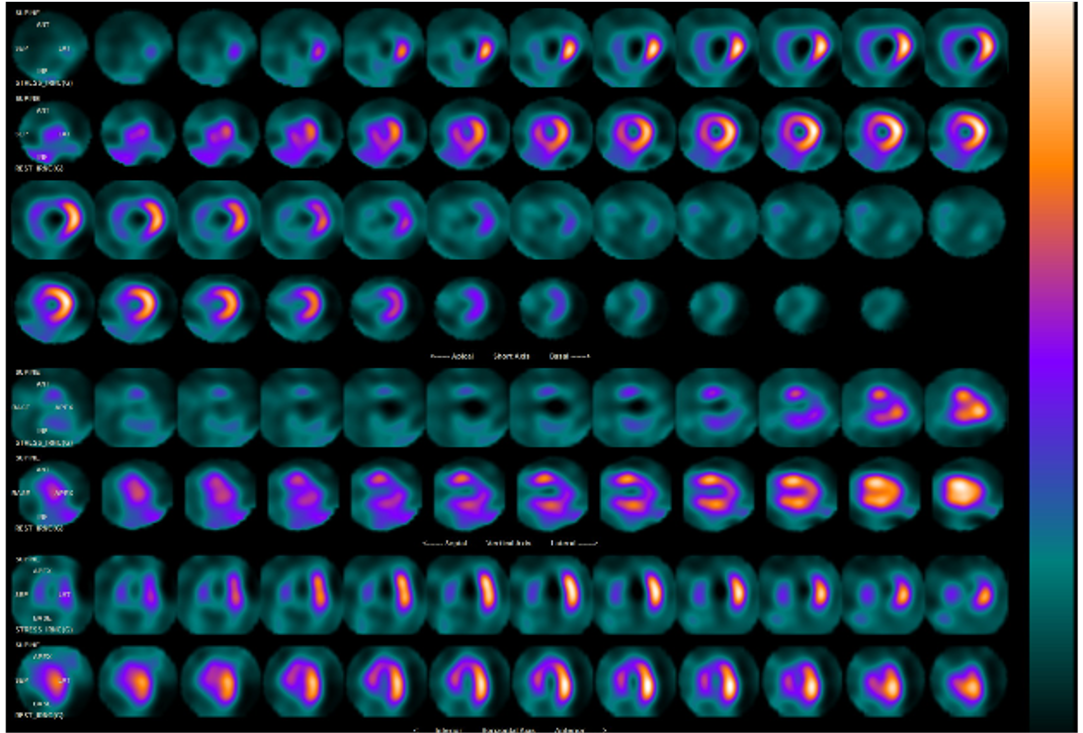
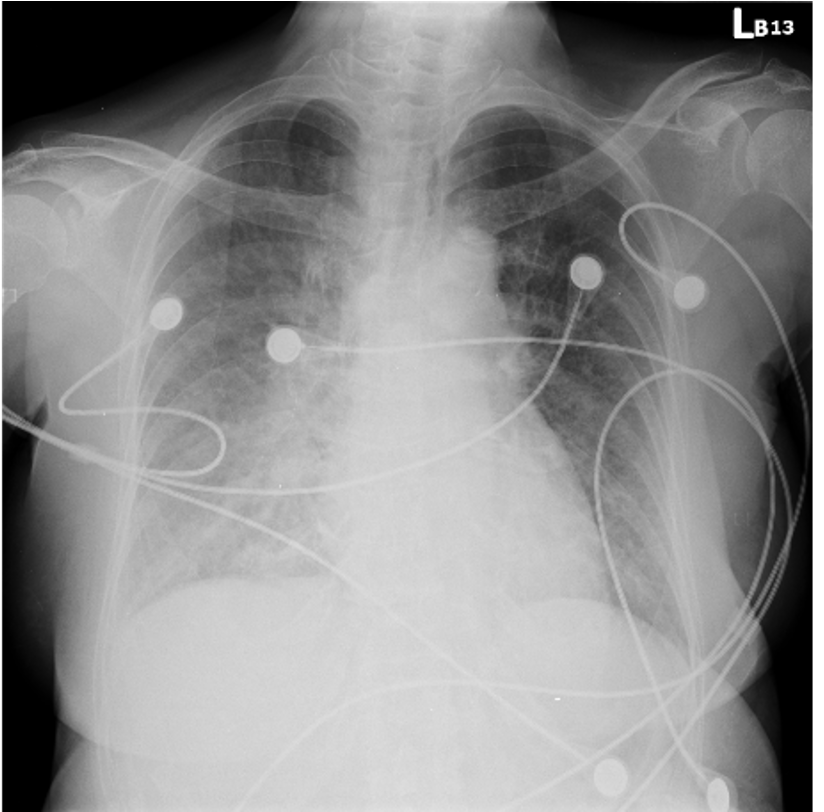
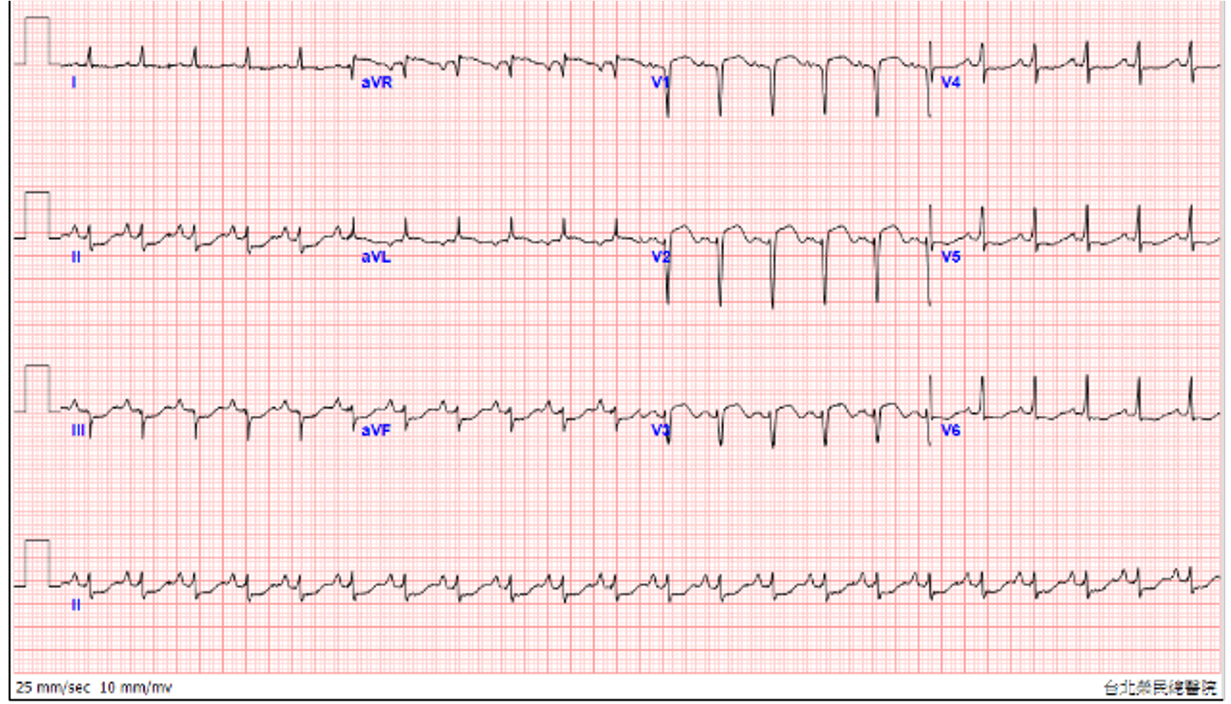
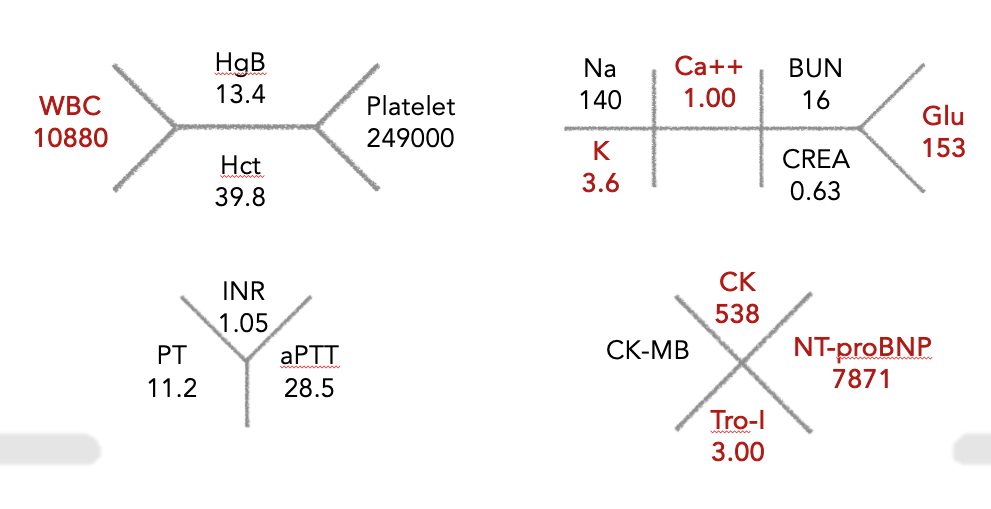
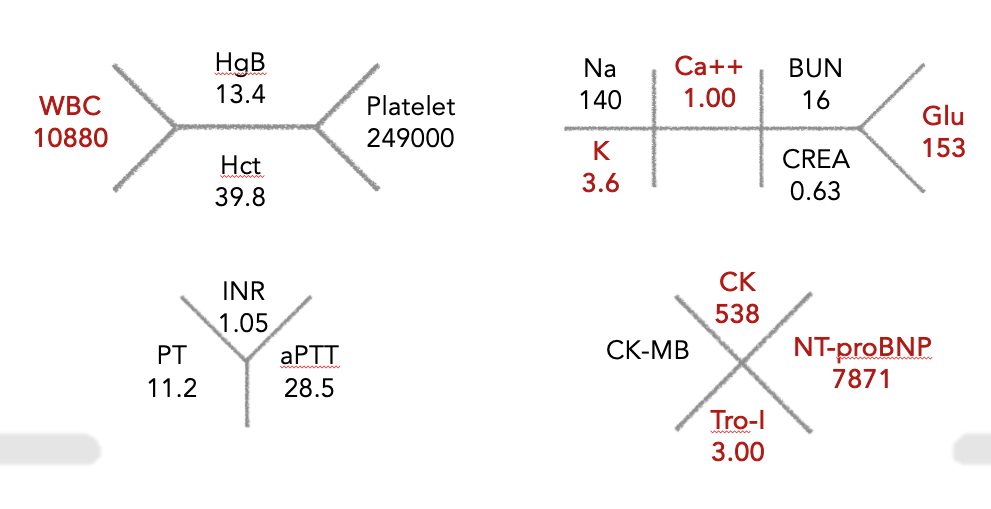
Relevant Test Results Prior to Catheterization
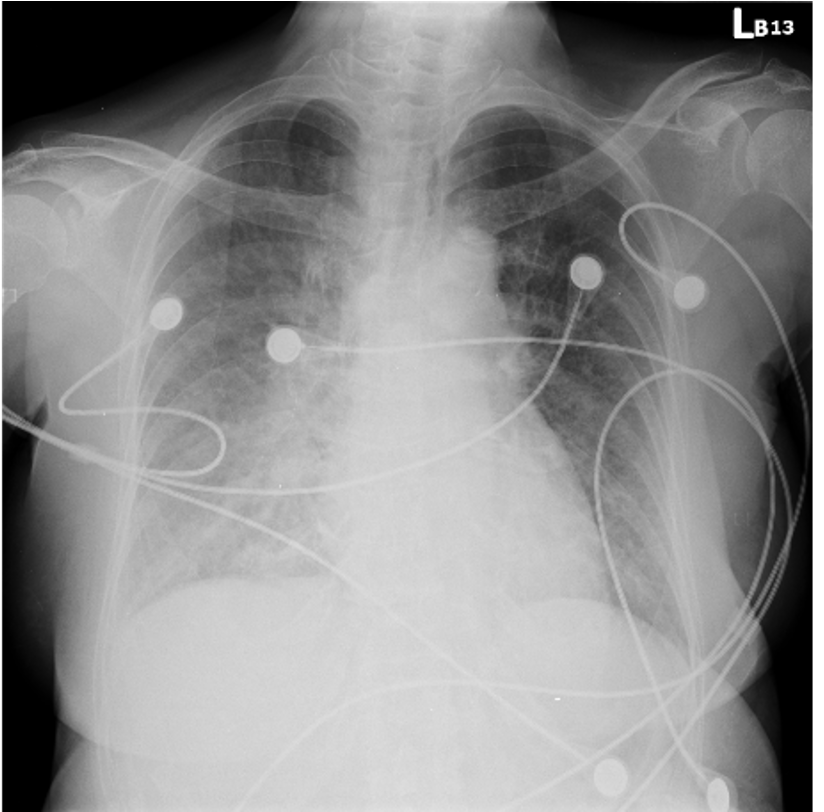
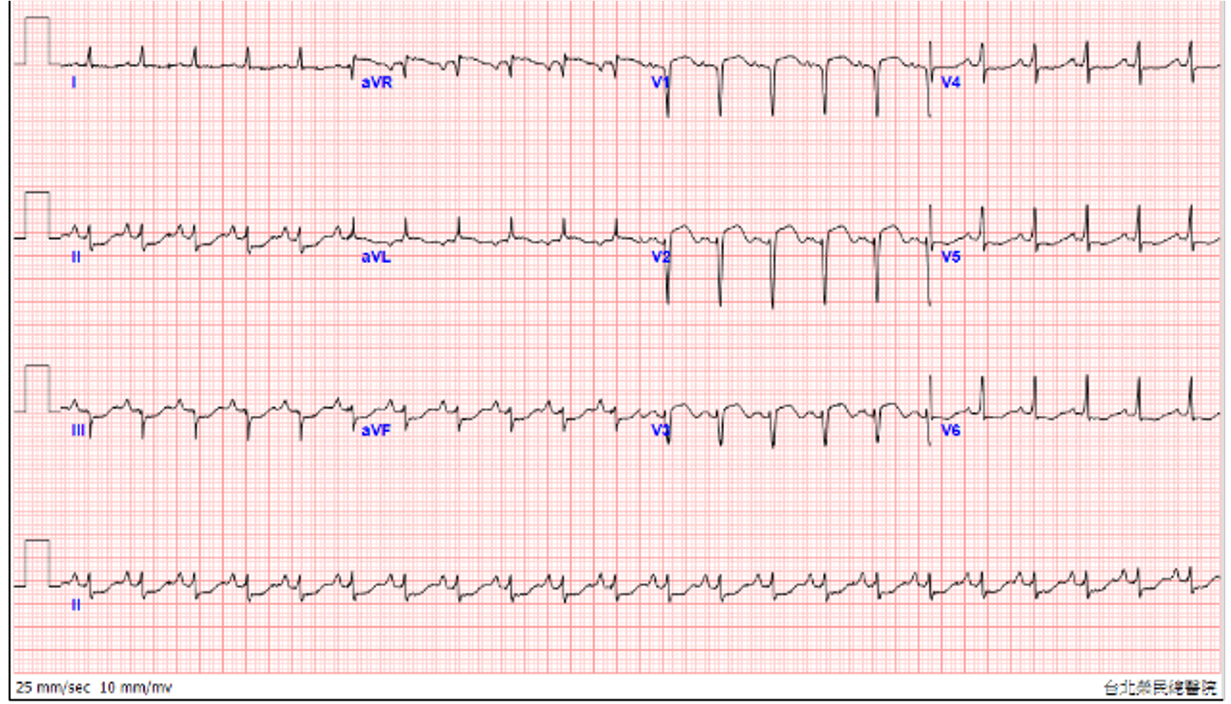
The CK and Tro-I initial level showed 538 U/Land 3.0 ng/mL, respectively, which was highly suspicious acute coronary syndrome. NTproBNP showed 7871pg/mL. Besides, at ED, the bedside echo showed antero-septal and antero-apical hypokinesis. The ECG showed precordial leads STE with reciprocal change. STEMI was impressed at that time. Also, CXR revealed acute pulmonary edema.
Relevant Catheterization Findings
The catheterization was performed via RRA with 6Fr sheath. We engaged RCA with JR 4/6 diagnostic catheter and found chronic total occlusion with collateral circulation from LAD septal and LCx. We then engaged LMCA with JL 3.5/6 diagnostic catheter and showed 90% severe stenosis with heavy calcified LM. LAD showed diffusely stenosis with heavy calcification from ostium to distal. LCx yielded diffusely stenosis up to 70% from ostium to middle.
 Caudal view_LM_bifurcation_lesion.mp4
Caudal view_LM_bifurcation_lesion.mp4
 Cranial view_LAD_heavy_Calcification.mp4
Cranial view_LAD_heavy_Calcification.mp4
 LAO view_RCA.mp4
LAO view_RCA.mp4
Interventional Management
Procedural Step
A EBU 3/6 guiding catheter was engaged to LMCA and advanced a Sion black guidewire to LAD-D. POBA was done with 2.0*15mm balloon pressure up to 14atm LAD-D to LM. Due to hypotension even under levophed pump, we inserted IABP from RFA. Further POBA was done with 3.0*15mm NC balloon pressure up to 12atm LAD-D to LM. However, at this time, unclear mental status was noted and persisted hypotension and bradycardia subsequently. Angiography showed LM dissection and LAD no reflow. Monitor showed PEA and CPCR started and we also activated ECMO team. After a few minutes CPCR, we continued our procedure after ECMO and intubation were initiated. IVUS showed diffuse and thickened calcification LAD-M to Os. Rotablation was indicated in this patient. We delivered a APT 2.6 Fr microcatheter to LAD-D and changed Sion black to Rota floppy GW. We advanced a Sion blue GW to LCX and removed microcatheter by trapping balloon technique. Rotablation was performed 6 times with 140000-180000 rpm. IVUS showed reverberation and cracked calcified plaque after rotablation. Further POBA was done with 2.0*15 and 3.0*15mm NC balloon LAD-M to LM pressure up to 14atm and 12atm, respectively. Due to bifurcation lesion, a Xience Xpedition 3.0*48mm DES was deployed at LM ostium to LAD M pressure, followed by post dilatation. Re-wiring was performed via distal stent strut and KBT was performed using 2.0*15 and 3.0*15mm balloon. POT was used over LM with 3.5*8mm balloon. The final angiogram showed TIMI3 flow.
 pre-ROTA_underexpansion.mp4
pre-ROTA_underexpansion.mp4
 Post-ROTA_well_expansion.mp4
Post-ROTA_well_expansion.mp4
 IVUS_360_Degree_heavy_calcification.mp4
IVUS_360_Degree_heavy_calcification.mp4
Case Summary
The final angiogram showed well-expansion stent with TIMI 3 flow. During intensive care unit, the patient regained her consciousness and weaned ECMO and intubation successfully. The patient discharge without any sequelae and followed at our out-patient clinic regularly.
