CASE20230825_008
When Stopping and Re-Attempt With Better Strategies Is the Best Option: Staging PCI in CTO With Heavy Calcified Lesions
By Mia Amira Callista, Amir Aziz Alkatiri, Doni Firman, Arwin Saleh Mangkuanom, Nanda Iryuza
Presenter
Mia Amira Callista
Authors
Mia Amira Callista1, Amir Aziz Alkatiri2, Doni Firman2, Arwin Saleh Mangkuanom2, Nanda Iryuza2
Affiliation
Tangerang Regional Hospital, Indonesia1, National Cardiovascular Center Harapan Kita, Indonesia2,
View Study Report
CASE20230825_008
Complex PCI - Calcified Lesion
When Stopping and Re-Attempt With Better Strategies Is the Best Option: Staging PCI in CTO With Heavy Calcified Lesions
Mia Amira Callista1, Amir Aziz Alkatiri2, Doni Firman2, Arwin Saleh Mangkuanom2, Nanda Iryuza2
Tangerang Regional Hospital, Indonesia1, National Cardiovascular Center Harapan Kita, Indonesia2,
Clinical Information
Relevant Clinical History and Physical Exam
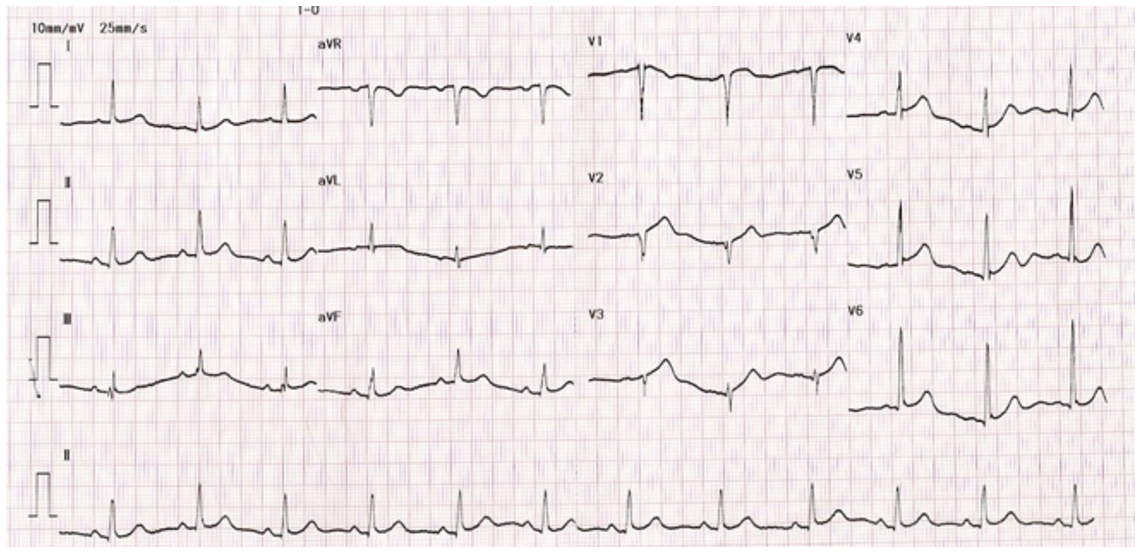
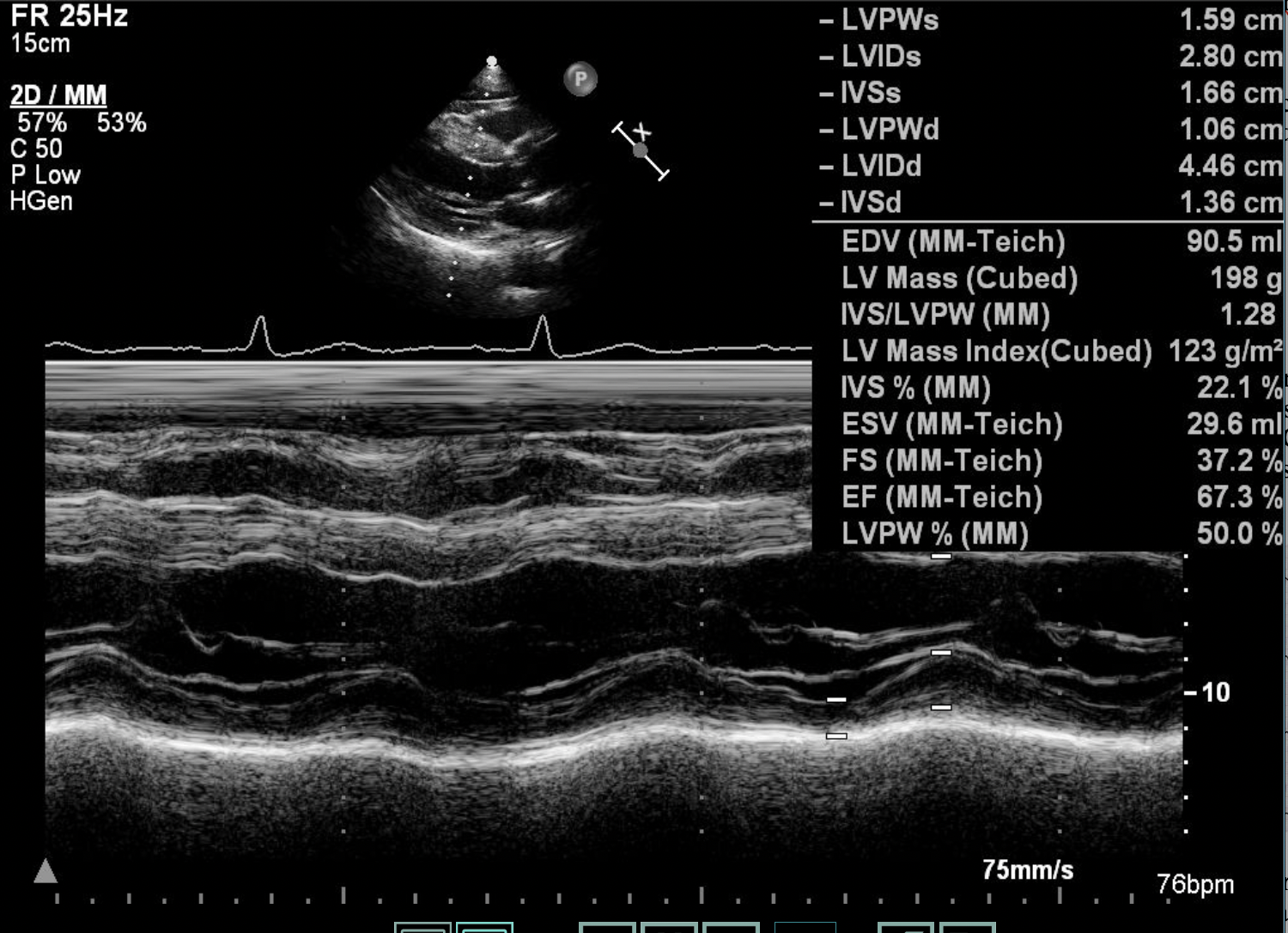
Relevant Test Results Prior to Catheterization
Echocardiography showed normal cardiac chamber size and normal Ejection Fraction. No regional wall motion abnormalities was seen and all of cardiac valves were normal. His chest-ray and blood test laboratories finding were within normal range.
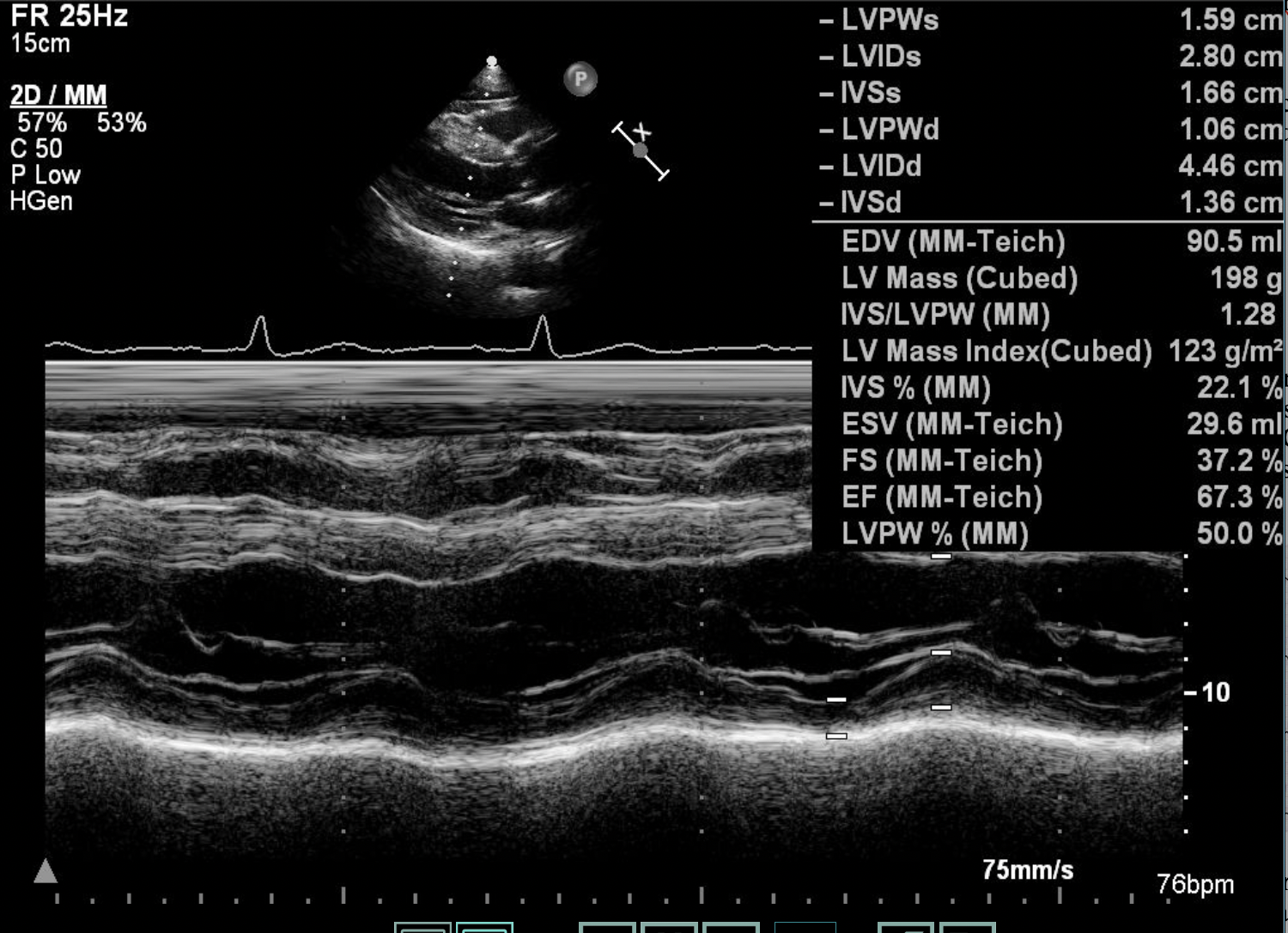
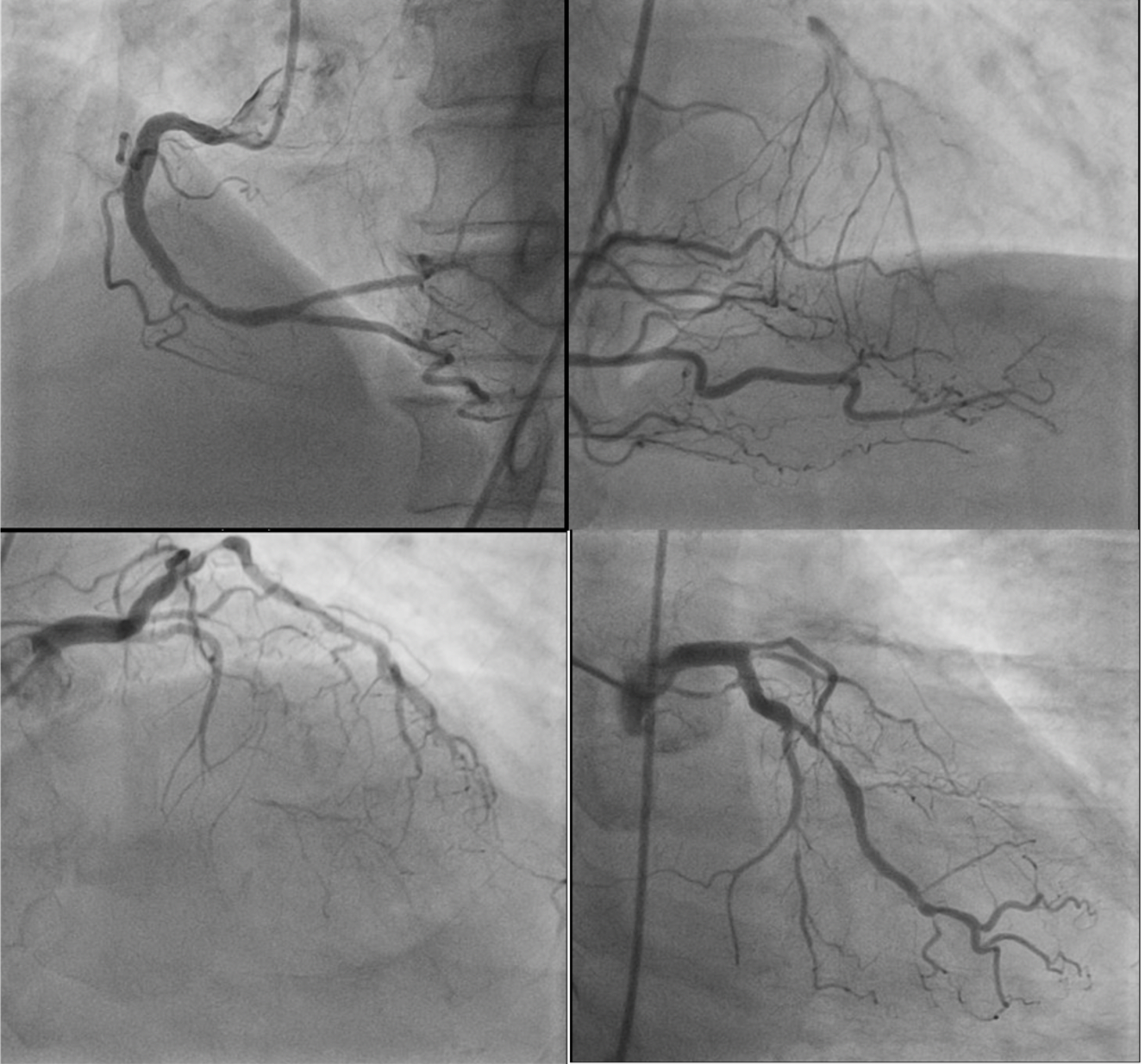
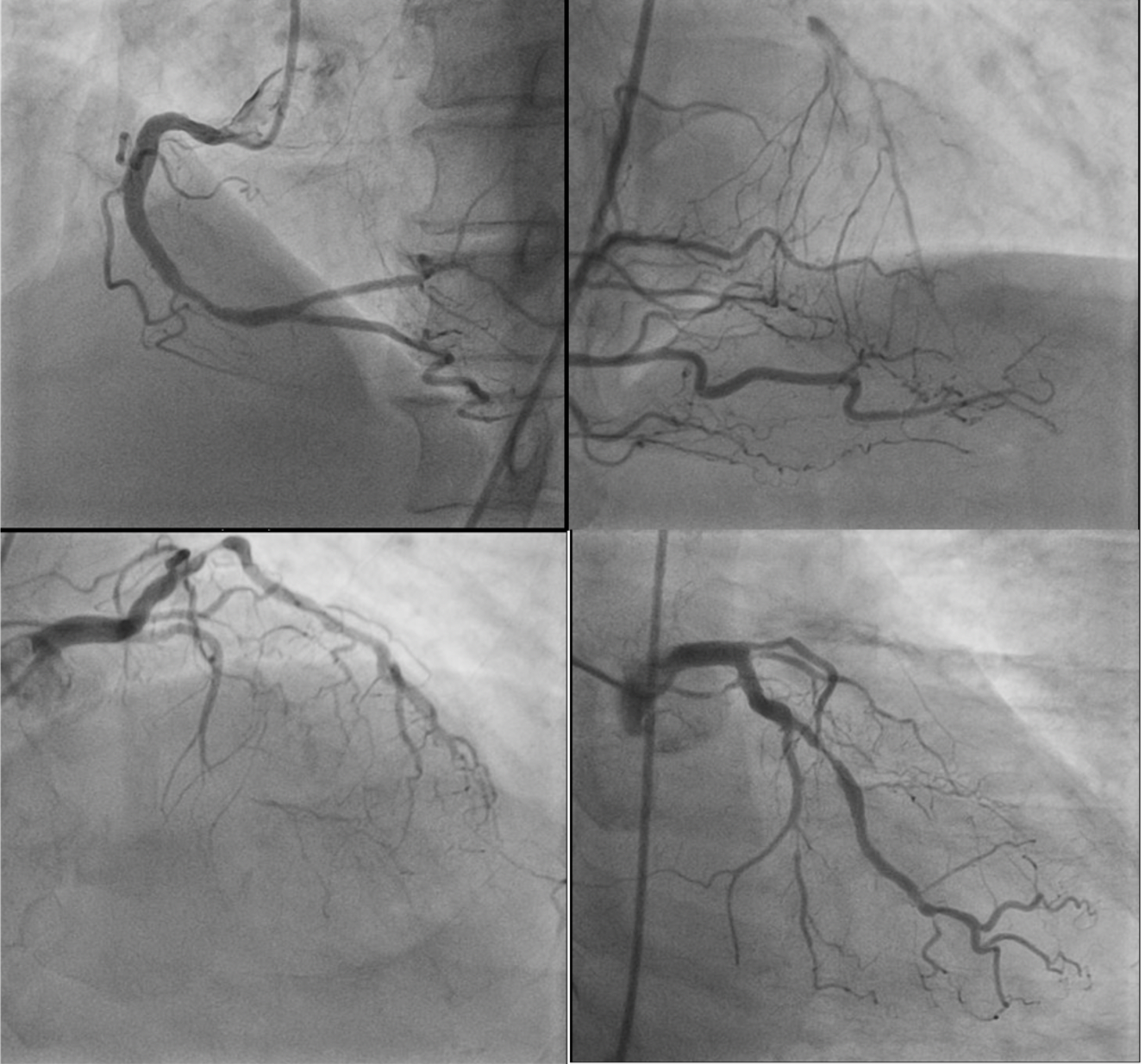
Relevant Catheterization Findings
Left Main Coronary Artery: Normal
Interventional Management
Procedural Step
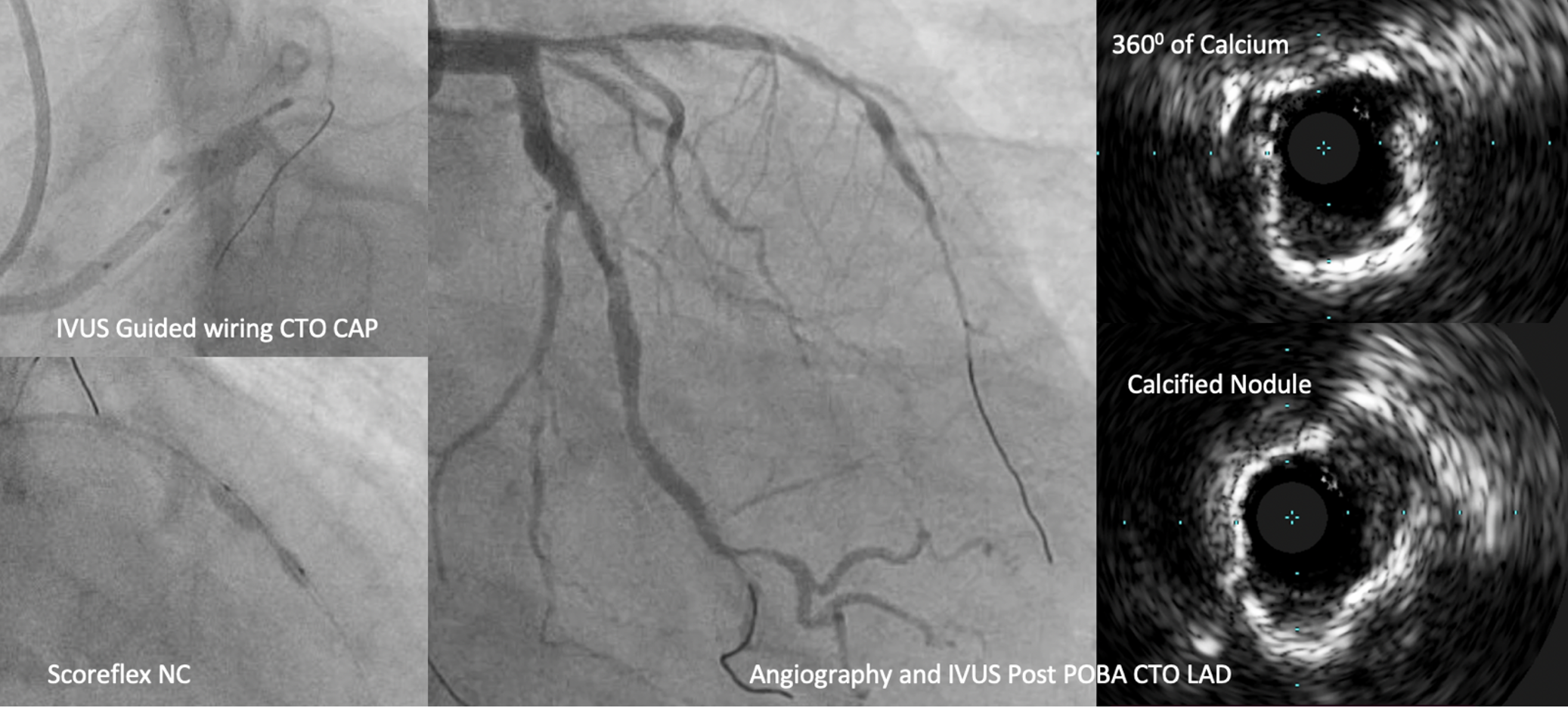
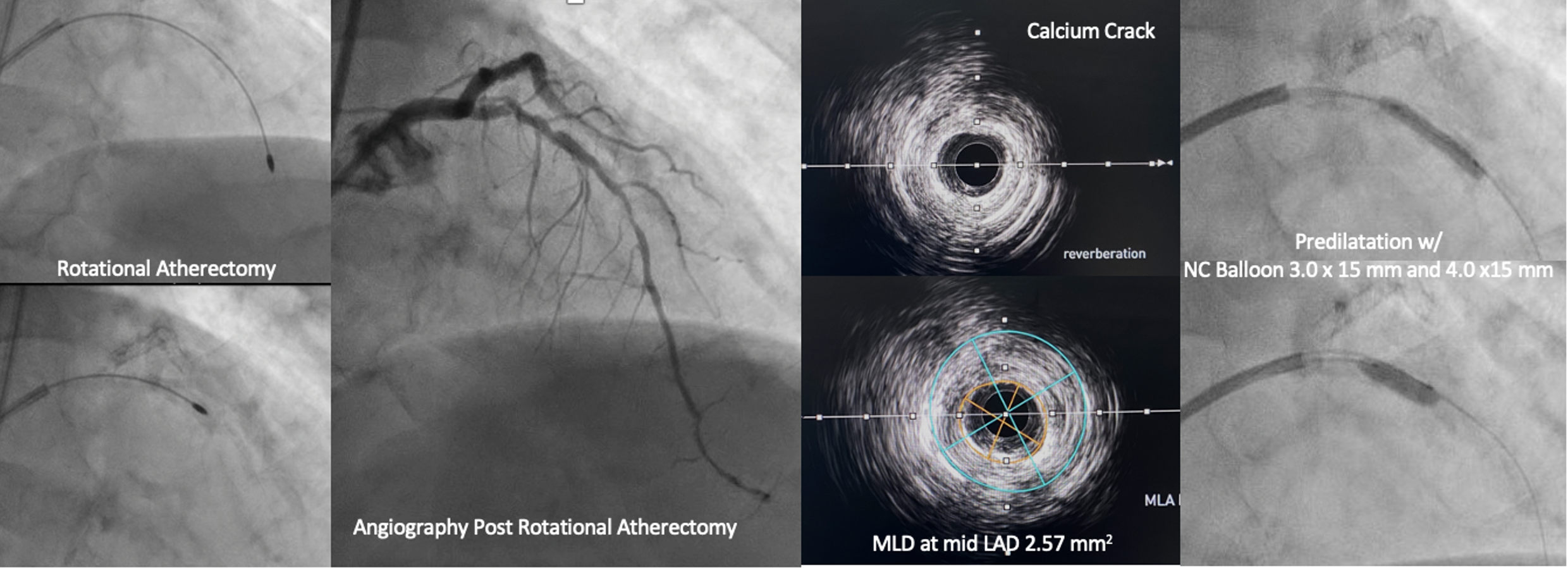
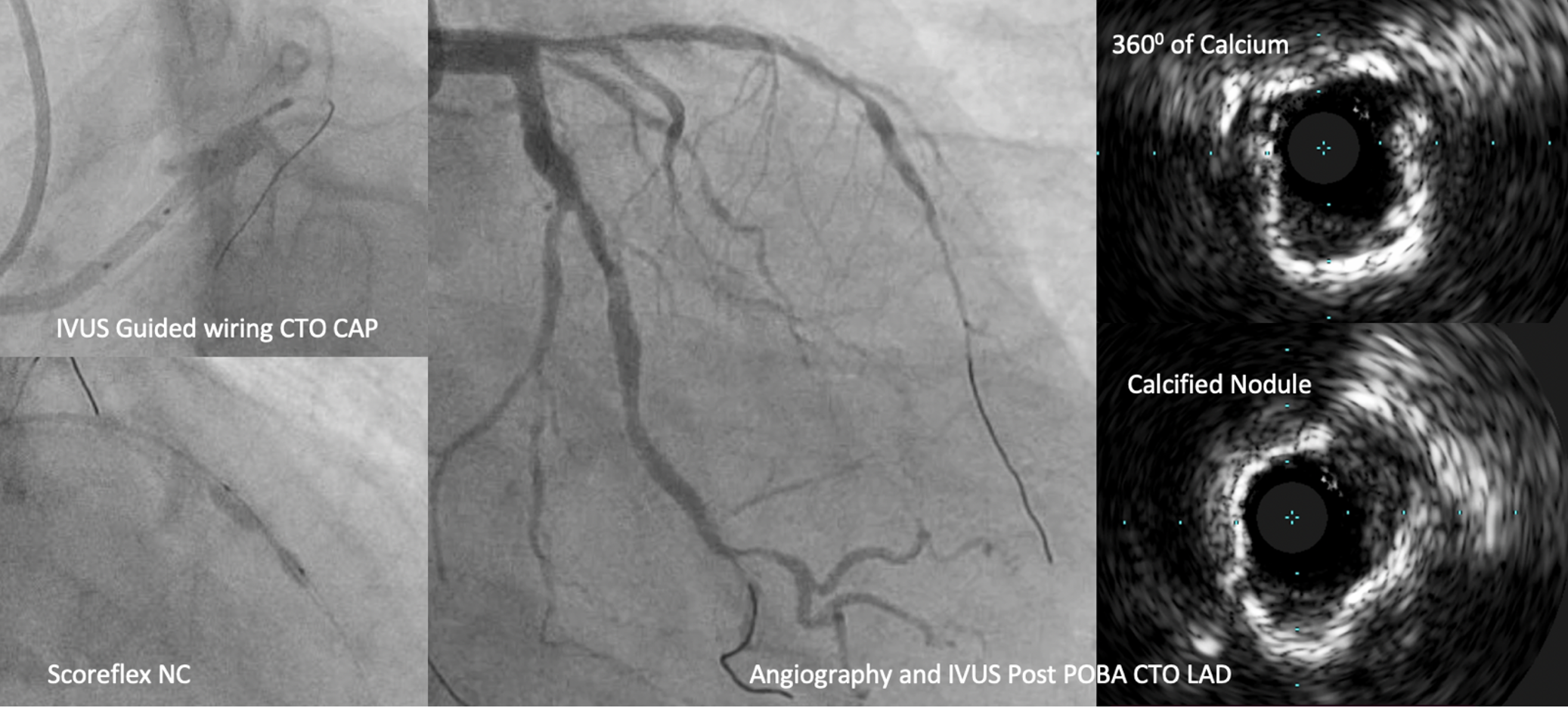
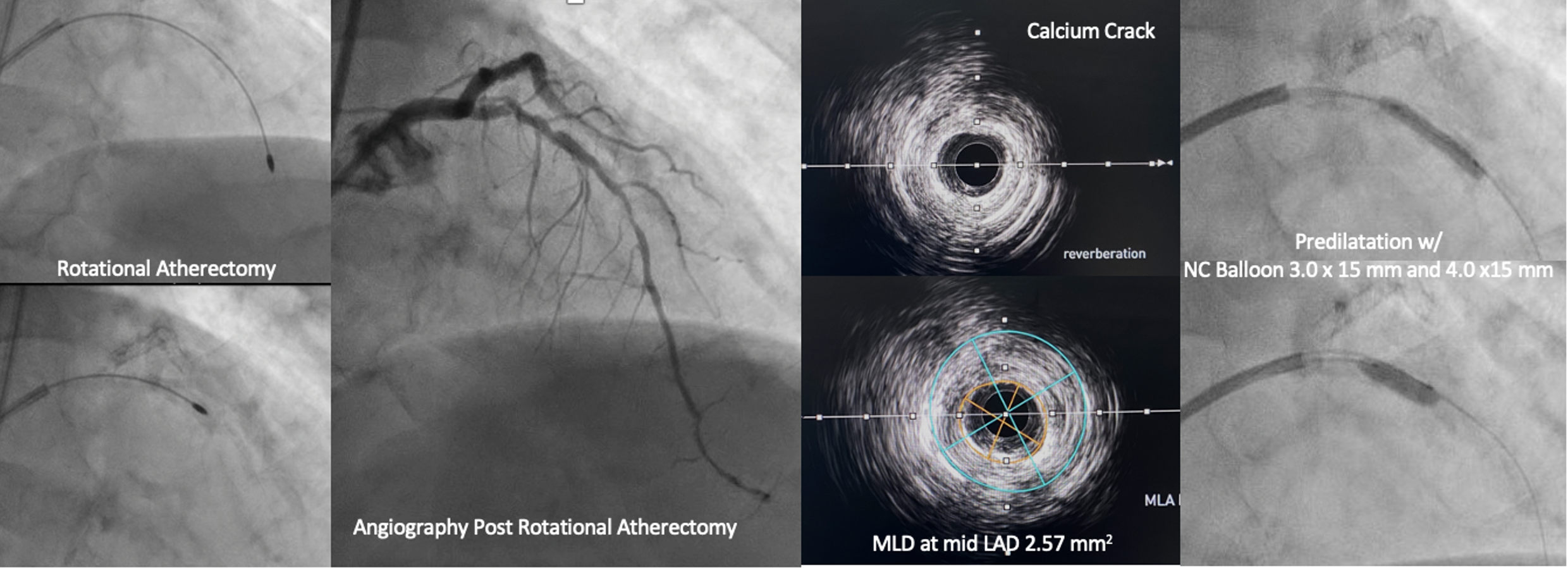
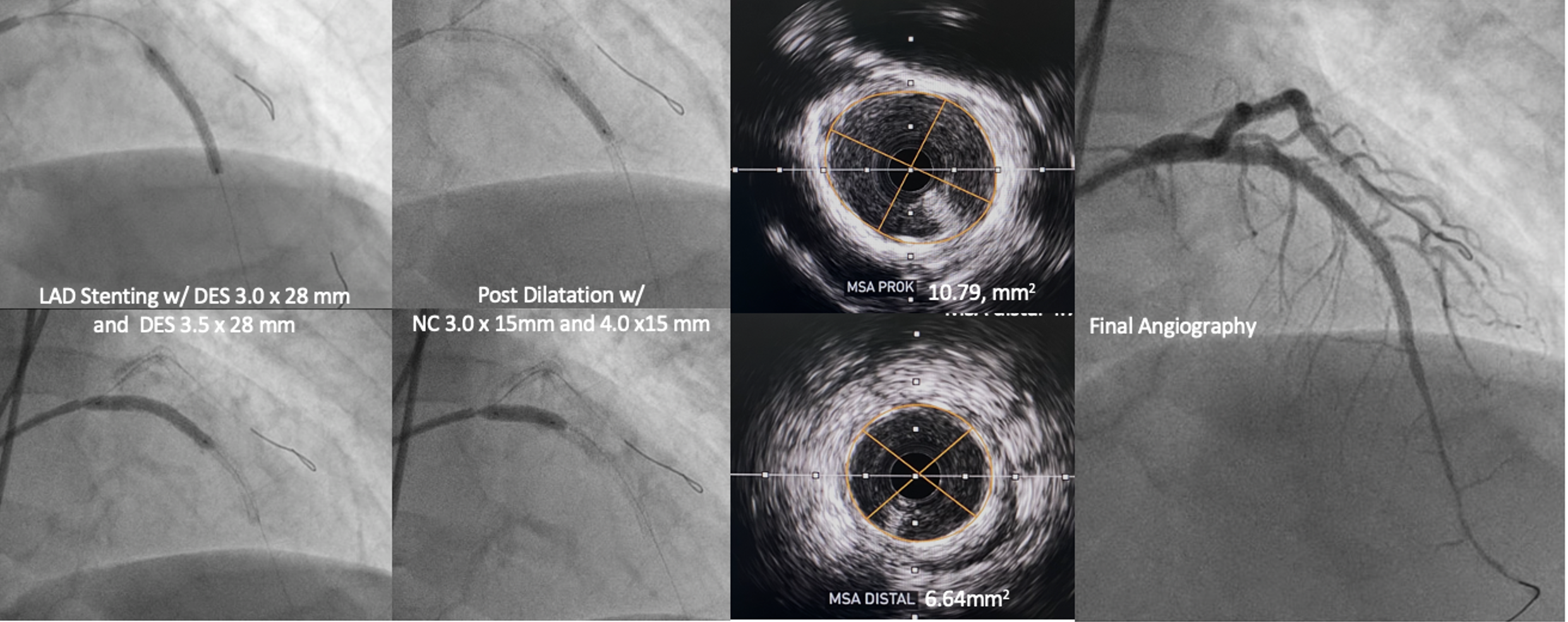
We performed PCI with dual injection strategy, guide catheter XB 3.5/8F on right femoral and JR 3.5/6F on right radial. IVUS guided was used to determine entry cap of osteal LAD. CTO was successfully crossed using wire Asahi Gaia Next III with microcatheter. Predilatation performed using semi compliant balloon 1.0 x 10 mm escalated to 2.5 x 15 mm. IVUS of LAD showed severe calcified plaque, calcified nodule and napkin ring (IVUS Calcium Score 3). We tried Scoreflex NC ballon 2.5 x 15 mm to modified the plaque, but it wasn’t fully expanded (24 atm). Angiography showed TIMI 3 Flow LAD with multiple non flow limiting dissection. We decided to stop PCI at LAD and proceeded PCI at LCx with DES 3.0 x 38 mm. Two months later, we reattempted PCI with Rotational Atherectomy. LCA was cannulated with XB 3.5/7F, angiography showed severe calcified LAD with no visible dissection. Rotational atherectomy was performed with a 1.5 mm burr up to 200000 rpm. Post-atherectomy IVUS showed calcium crack, distal reference lumen diameter 3.14-3.55 mm and osteal LAD EEM 4.46-4.63 mm. Pre-dilatation was performed using scoreflex NC 2.5 x 15 mm and 3.5 x 15 mm. Proximal-mid LAD was stented with DES 3.0 x 28 mm (16 atm), and osteal LAD using DES 3.5 x 28 mm (16 atm). We optimized stent expansion with NC balloon 3.0 x 15 mm (20 atm) mid LAD and NC 4.0 x 15 mm (20 atm) osteal-proximal LAD. Final IVUS showed stent well apposed and well expanded with no dissection (MSA distal 6.64 mm2, Proximal 10.79mm2).
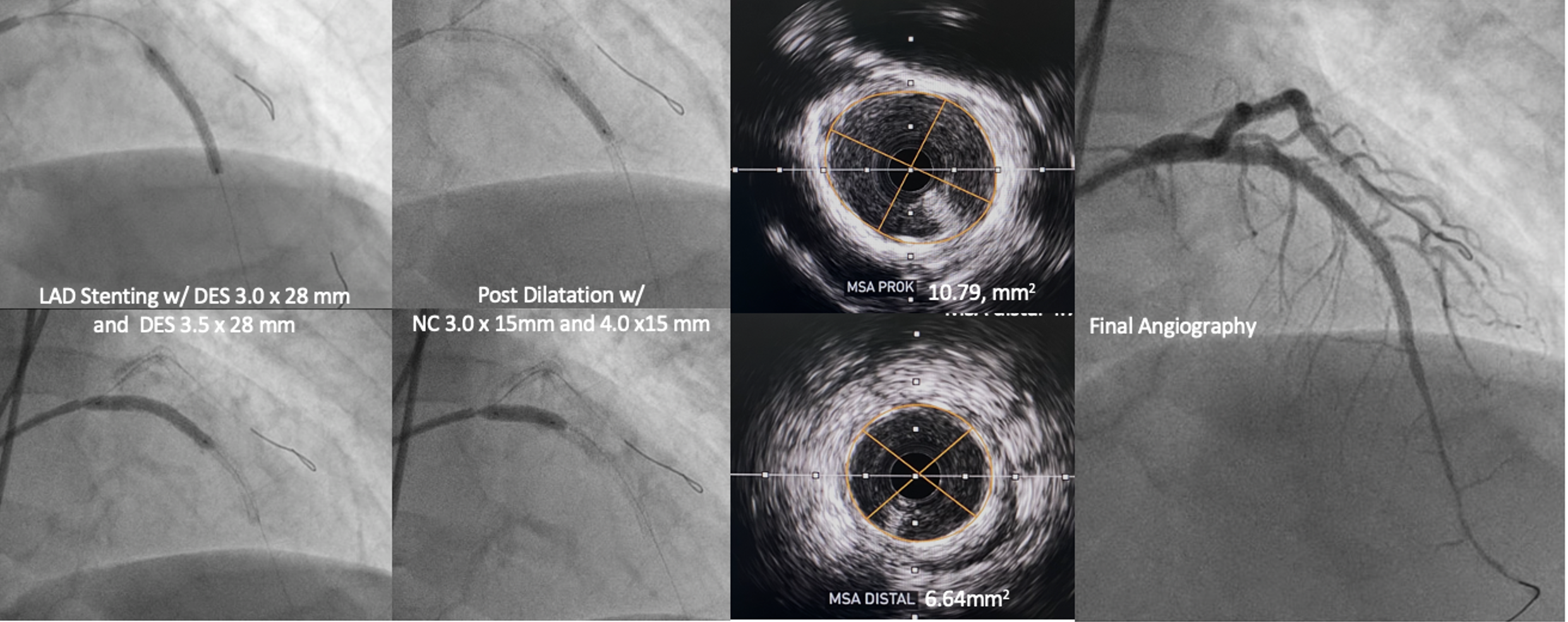
Case Summary
When a procedure cannot be performed as planned, we need to step backward, reanalyse, and always be prepared with plan B. In this case, we experienced the challenge of CTO with ambiguous cap with unexpected severe calcified lesion. When the CTO was successfully crossed yet Scoring NC balloon could not be fully inflated and dissections were seen, we decided to stop the procedure. We changed the strategies and reattempt PCI using rotational atherectomy for optimal plaque preparation after the dissections were healed.
