CASE20230825_007
Complications of Heparin-Induced Thrombocytopenia in the Post-Emergency Bentall Procedure: Frequent Circuit Changes in V-A ECMO due to Massive Thrombosis
By Nao Yasuda, Tsuda Takuma
Presenter
Nao Yasuda
Authors
Nao Yasuda1, Tsuda Takuma1
Affiliation
Nagoya Ekisaikai Hospital, Japan1,
View Study Report
CASE20230825_007
Complication Management - Complication Management
Complications of Heparin-Induced Thrombocytopenia in the Post-Emergency Bentall Procedure: Frequent Circuit Changes in V-A ECMO due to Massive Thrombosis
Nao Yasuda1, Tsuda Takuma1
Nagoya Ekisaikai Hospital, Japan1,
Clinical Information
Relevant Clinical History and Physical Exam
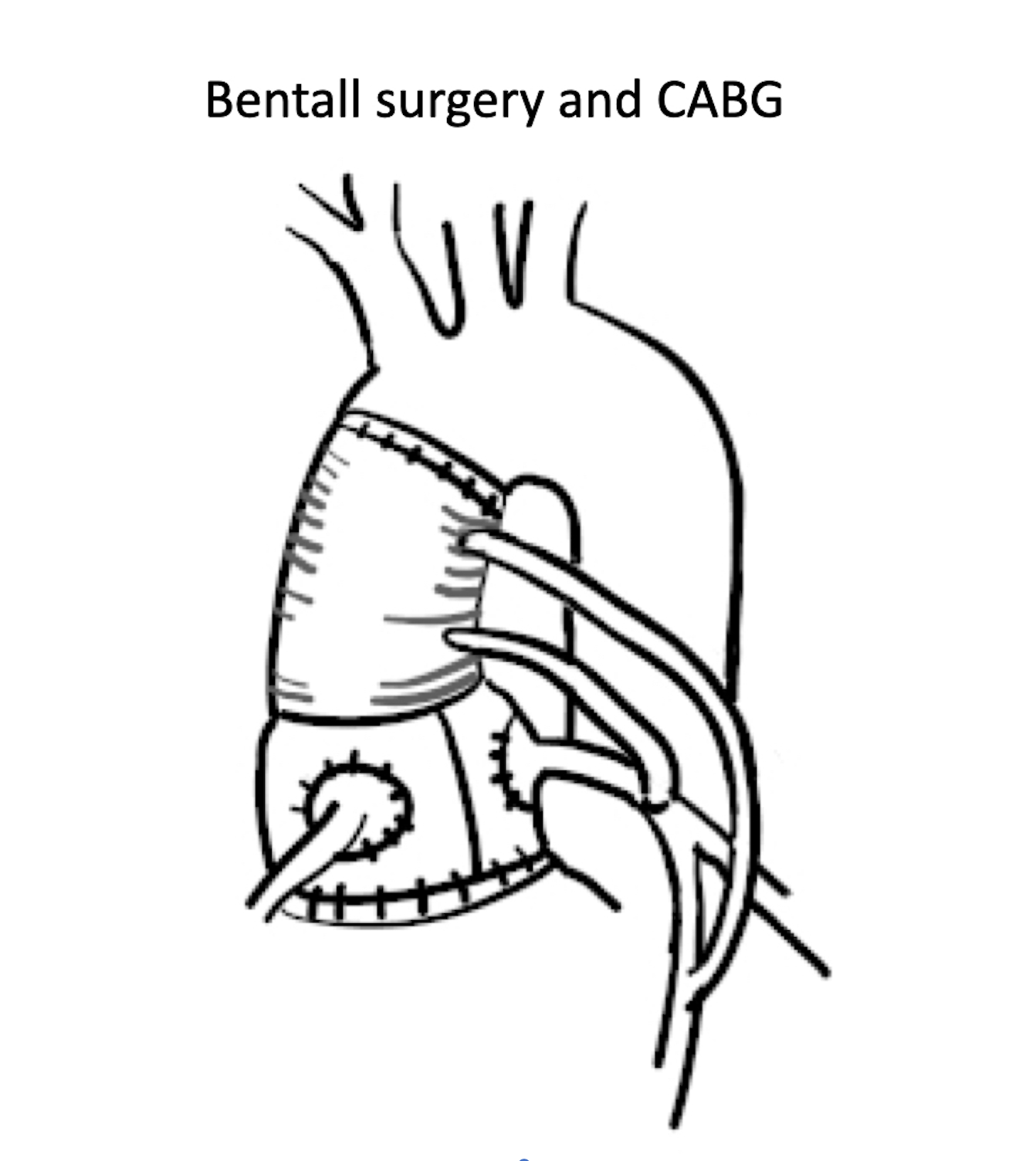
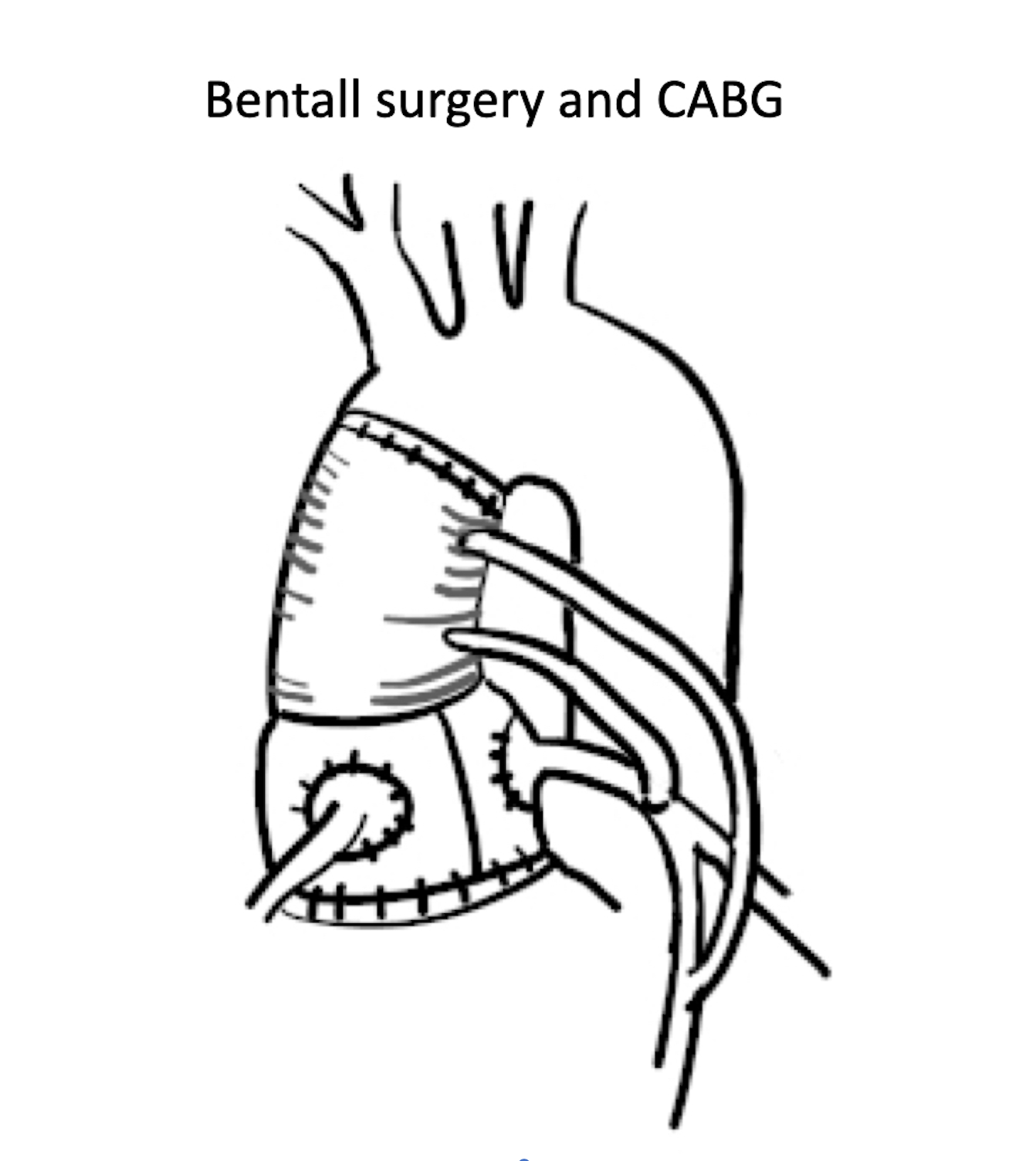
A 40-year-old male. He underwent emergency Bentall surgery due to acute type A aortic dissection, in addition to CABG procedures involving SVG-LMT and SVG-LAD. He was discharged from the intensive care unit on the 13th day and was progressing well with rehabilitation. However, on the 19th day of hospitalization, he suddenly developed ventricular fibrillation and V-A ECMO was inserted. Emergency coronary angiography was performed.
 CT.mp4
CT.mp4
Relevant Test Results Prior to Catheterization
The Relevant test results prior to the sudden change are as follows.The electrocardiogram showed sinus rhythm with non-specific ST changes.The echocardiogram: EF 56%, IVSd 10.8mm, LVID 42.0mm, LVPWd 10.3mm, LVIDs 27.5mm. Minimal tricuspid valve leaflet (TVL) movement observed in the A valve, and mild hypokinesis from the base to the anterior wall extending to the lateral wall was observed. A small amount of pericardial effusion was present.
Relevant Catheterization Findings
In the emergency coronary angiography, a 100% occlusion was observed in the SVG-LAD that had been reconstructed through CABG, leading to the diagnosis of Acute Coronary Syndrome (ACS).
 pre_0001.mp4
pre_0001.mp4
 ivus_0001.mp4
ivus_0001.mp4
Interventional Management
Procedural Step
IVUS revealed a large amount of red thrombus, and successful revascularization was achieved through the placement of a DES (Xience Skypoint 4.0/12) in the SVG-LAD, which had been reconstructed through CABG. Platelet count had decreased drastically to 2,200/μl in a blood sample taken just before the PCI procedure. Abnormalities in systemic blood pressure were observed since the initiation of ECMO, and on the 20th day of hospitalization, there was an increase in artificial lung inlet pressure leading to a loss of flow. As a result, the ECMO circuit exchange was performed, but on the 21st day, an abrupt emergency stoppage of ECMO occurred again. Upon detaching the circuit for exchange, it was found that the lumen of the arterial cannula was occluded by a thrombus. Due to frequent circuit exchanges caused by thrombosis and the decrease in platelet count during critical events, heparin-induced thrombocytopenia (HIT) was suspected. Heparin was discontinued and anticoagulation was initiated using nafamostat mesylate and argatroban. However, on the 22nd day, a significant amount of thrombus was once again observed in the artificial lung, leading to a switch to a circuit without heparin coating. Despite these measures, the platelet count did not increase, multiple organ failure progressed, and The patient passed away on the 28th day. HIT antibodies tested positive.
 final_0001.mp4
final_0001.mp4

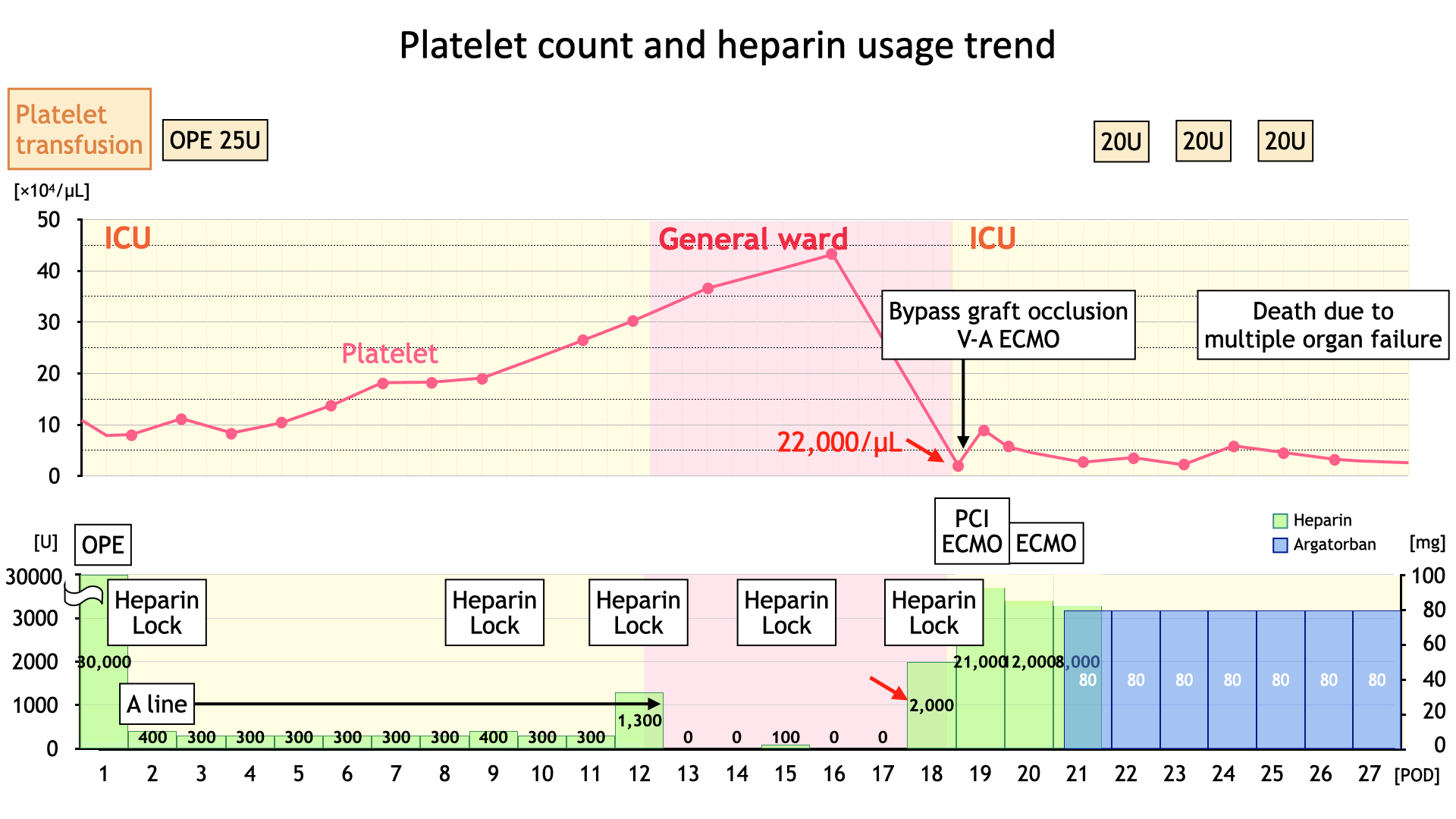

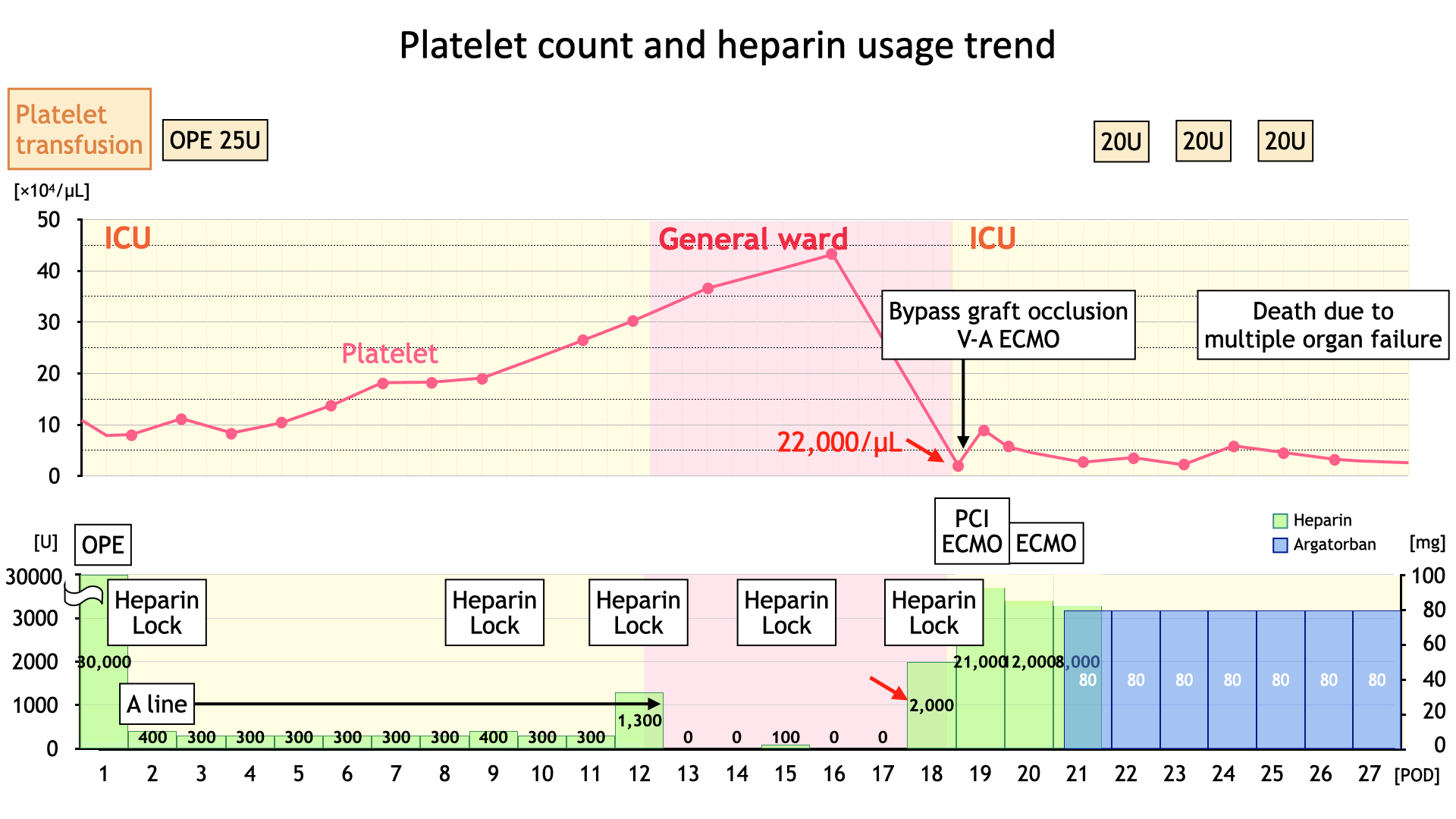
Case Summary
In this case, at the 14th day of hospitalization, there was no observed decrease in platelet count. However, on the morning of the 18th day, the rapid progression of HIT was believed to have been triggered by the heparin lock introduced through a peripheral vascular route. It's been reported that cardiac surgery can result in HIT in around 2% of cases, and since it can lead to fatal complications, it is crucial to always consider the possibility of HIT in cases of ACS following cardiac surgery.
