Good PCI Planning with Drug-coated Balloons and FFR Can Limit Long Stents for Diffuse Long CA
Antonio Colombo, MD, calls for shift in planning and angioplasty strategy when stenting complex lesions
Long stents in diffuse long coronary artery disease (CAD) may be the gut reaction for cardiologists during complex percutaneous coronary intervention (PCI), but a more refined approach can help limit stent length and improve outcomes.
 "Stenting is appropriate in certain cases such as focal lesions with high peak-to-peak gradient (PPG), but stent implantation cannot be the default approach for all coronary stenosis," said Antonio Colombo, MD (Humanitas Research Hospital, Rozzano, Italy) at COMPLEX PCI 2021 Virtual on Nov. 25." Contemporary interventional cardiology can't translate to PCI for all lesions."
"Stenting is appropriate in certain cases such as focal lesions with high peak-to-peak gradient (PPG), but stent implantation cannot be the default approach for all coronary stenosis," said Antonio Colombo, MD (Humanitas Research Hospital, Rozzano, Italy) at COMPLEX PCI 2021 Virtual on Nov. 25." Contemporary interventional cardiology can't translate to PCI for all lesions."
"The immediate results of PCI may be perfect, but it's not rare to see total occlusion with long stents a few years down the road," he added. "Not all coronary stenosis is the same, and angiography isn't always the best tool for decision making. It's also important to distinguish between malignant and benign dissections."
Presenting what Alan C. Yeung, MD (Stanford University School of Medicine, California, USA) called an "innovative" approach to limit stent length where "long stents and worse outcomes are typical," Colombo outlined when and when not to use long stents.
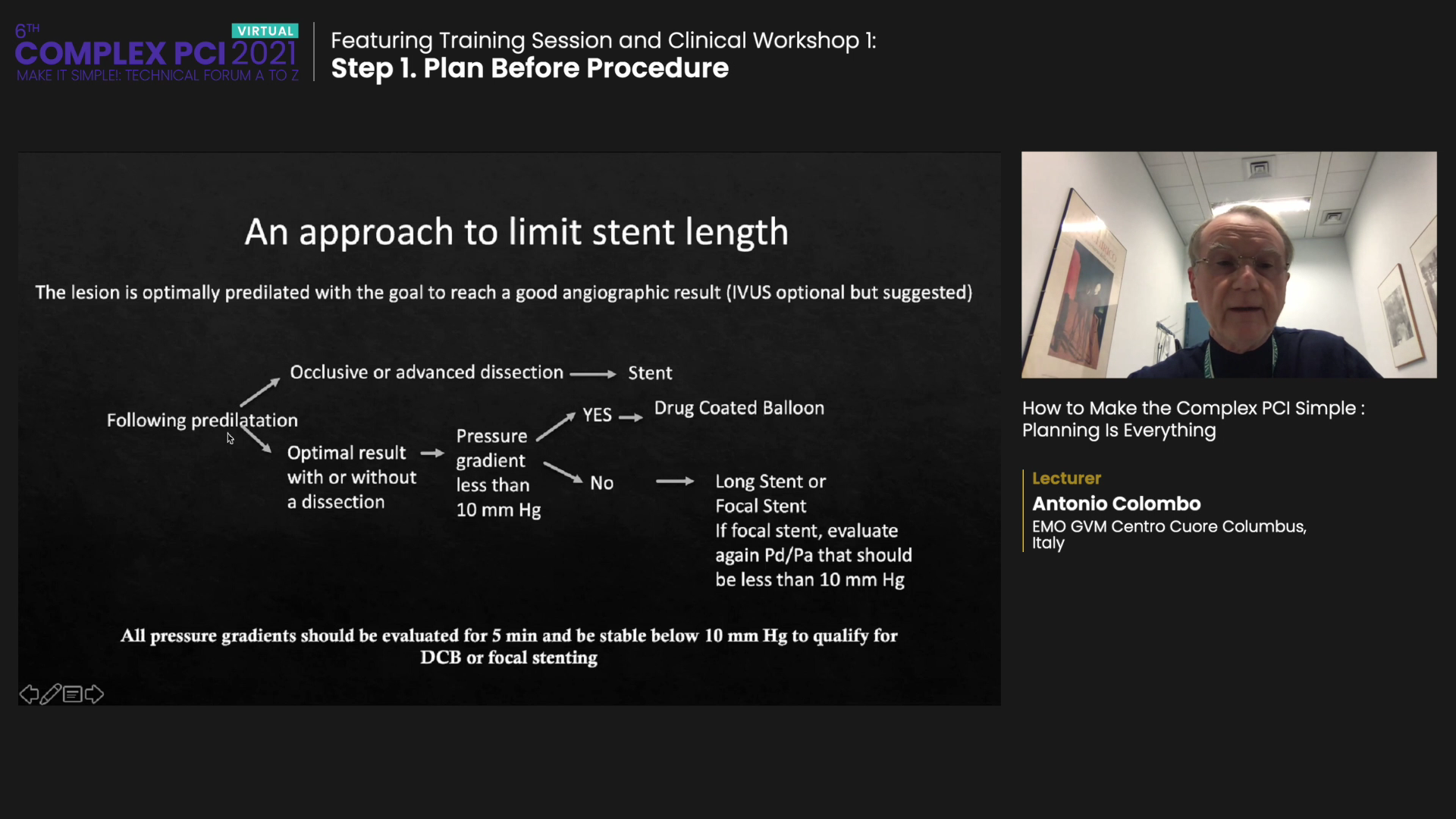
According to the approach, stenting is appropriate for occlusive or advanced dissection performed after predilation with intravascular ultrasound (IVUS). However, drug-coated balloons (DCB) should be used in predilated cases where the pressure gradient is less than 10 mmHg, and an optimal result can be achieved regardless of dissection. Long or focal stents can be used when the pressure gradient exceeds 10 mmHg, and an optimal result is possible with or without dissection.
All pressure gradients should be evaluated for 5 minutes and be stable (<10 mmHg) to qualify for DCB or focal stenting.
"This approach," Colombo said, "is not necessarily to prevent restenosis, which can occur after stenting, but to make coronary disease treatment more physiologically apt in the long term. Drug-coated balloons with FFR evaluation can limit stent length."
Long diffuse coronary lesions (>20 mm) have traditionally posed a challenge to cardiologists due to their risk of in-stent restenosis and poor outcomes. Diffuse CAD accounts for around 20 percent of PCI cases1 and refers to multiple stenoses or long-segment occlusions in the heart.
The complex condition requires high expertise of the operator as well as multiple stents that raise the risk of complications such as high medication dosage, overlapping stents, and vascular injury that can lead to restenosis and late stent thrombosis. The lesion length is also known as an independent predictor of in-stent restenosis, especially in the era of bare-metal stents (BMS).
PCI for all lesions can't be contemporary interventional cardiology because not all stenosis is the same.
Due to disease complexity, diffuse long CAD reports a higher risk of reoccurring coronary symptoms such as stent thrombosis and restenosis after PCI. Some studies show symptom reoccurrence in 20-30 percent of patients2.
Drug-eluting stents (DES), a new advancement in the PCI landscape, overcame many of the limitations associated with BMS to produce better outcomes and surface as a reasonable strategy for diffuse long CAD. Longer DES stents (>33 mm) can reduce the risk of stent overlap when treating long lesions for better outcomes.
However, the variety of 38 mm stents on the market and the fact that very long lesions still require multiple stents have confounded cardiologists looking for the correct stenting strategy.
Colombo called for a shift in planning and angiography strategy, considering the rate of in-stent restenosis remains relatively high despite dropping to 5 to10 percent in the DES era.3
Generally, the default approach for complex PCI is to put in short stents (<25 mm) in large vessels (>3 mm) with optimized imaging. Stents with imaging optimization are also used in complex PCI with diffuse long coronary disease, including total occlusion.
However, Colombo stressed that "not every dissection requires stenting, indicating the necessity of evaluating malignant and benign dissections and DCB's pressure gradient."
Notably, drug-coated balloons paired with repeat physiological assessment with the Pd/Pa ratio (coronary pressure/aortic pressure) and FFR could comprise a good planning strategy that allows optimal lesion preparation and limits stent length.
An observational trial is underway to examine proximal stenting and distal DCBs for reducing the need for a full metal jacket with a case series completed hopefully by next year, Colombo said.

