DKCRUSH-V vs. EBC MAIN Analysis ĄŪCasts ShadowĄŊ on Provisional Stenting Benefits for Complex LM
Shaoliang Chen, MD cautions against drawing ĄŪriskyĄŊ conclusions by choosing stepwise provisional stenting for complex left main bifurcation
Findings from the EBC MAIN trial published earlier this year may raise troubling implications if it prompts broad selection of provisional single stenting over the upfront double-stent technique in complex distal left main (LM), an expert said recently.
 Shaoliang Chen, MD (Nanjing Medical University, Jiangsu, China) at COMPLEX PCI 2021 Virtual on Nov. 26 called into question the applicability of EBC MAIN findings after comparing the study with the DKCRUSH-V trial, concluding that the higher rates of adverse events of provisional stenting (PS) in the former discourage extending results to the clinical setting.
Shaoliang Chen, MD (Nanjing Medical University, Jiangsu, China) at COMPLEX PCI 2021 Virtual on Nov. 26 called into question the applicability of EBC MAIN findings after comparing the study with the DKCRUSH-V trial, concluding that the higher rates of adverse events of provisional stenting (PS) in the former discourage extending results to the clinical setting.
Ą°Considering the analysis, the findings and comments raised in the paper could be risky if it stimulates interventional cardiologists to pursue the stepwise provisional single stent strategy for the majority of patients presenting complex lesions affecting the distal left main,Ąą Chen said.
Until DKCRUSH-V, provisional stenting was the most common strategy to treat unprotected distal LM bifurcation lesions in patients undergoing percutaneous coronary intervention (PCI).
DKCRUSH-V findings showed the upfront double-stent strategy (DK Crush) produced better results than provisional stenting. The multicenter, randomized trial conducted on 486 patients with unprotected LM distal bifurcation lesions (Medina 1,1,1 or 0,1,1) in five countries1 was the second significant randomized trial to pit PS (n=242) against DK Crush (n=240).
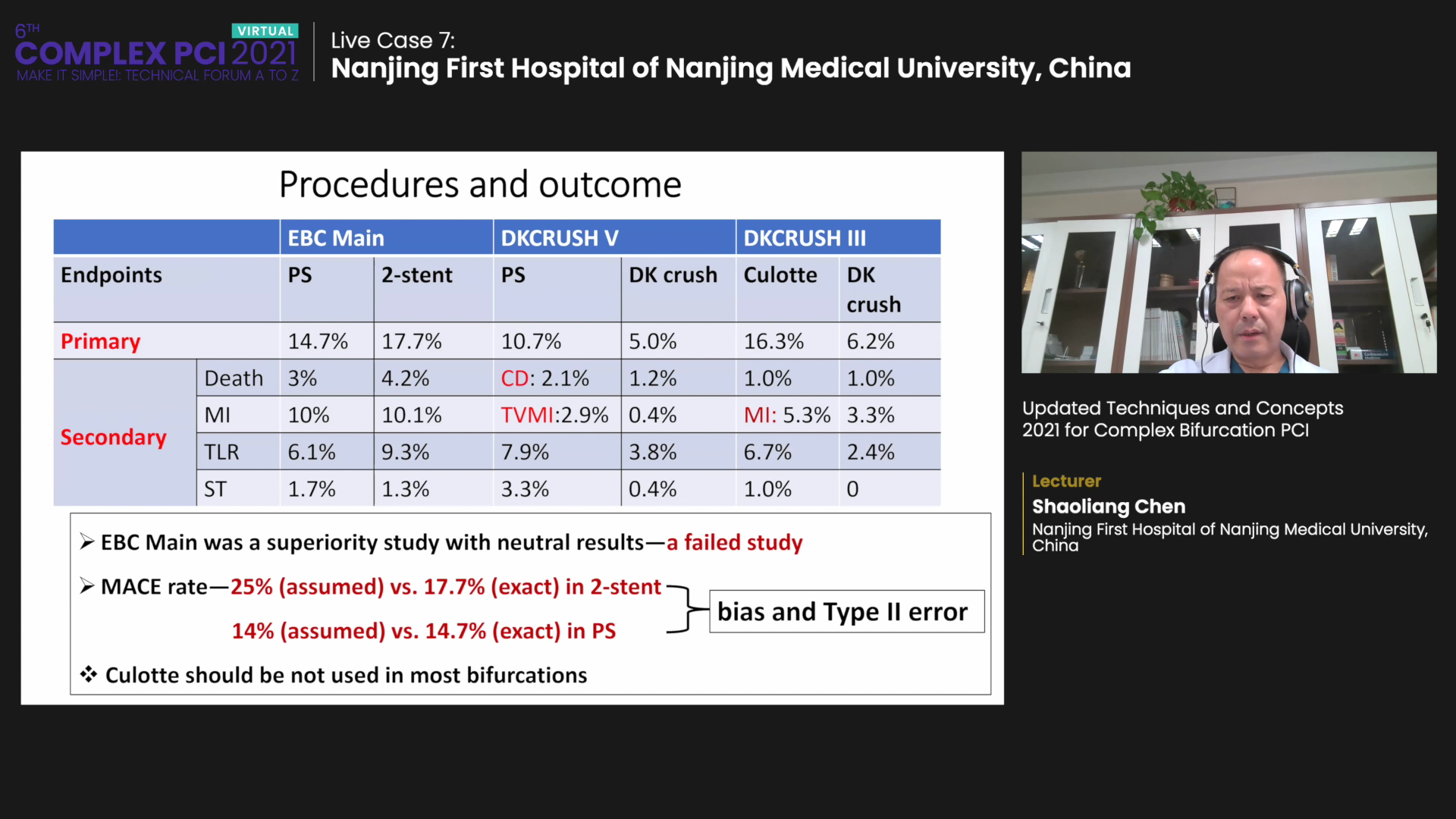
DKCRUSH-V found the upfront two-stent strategy lowered the incidence of 1-year target lesion failure (10.7% vs. 5.0%, HR 0.42, 95% CI, 0.21-0.85, p=0.02), target vessel myocardial infarction (2.9% vs. 0.4%, p=0.03), and definite/probable stent thrombosis (3.3% vs. 0.4%, p=0.02).
DK Crush also lowered rates of clinically driven target lesion revascularization (7.9% vs. 3.8%, p=0.06) and angiographic restenosis in the LM complex (14.6% vs. 7.1%, p=0.10). Cardiac death rates were similar in both groups. Similar findings were found in the 3-year follow-up on target lesion failure (TLF) in 20192.
DKCRUSH-V results set the groundwork for the 2018 European Society of Cardiology (ESC) Guideline on Myocardial Revascularization to level a Class IIb recommendation on the upfront two-stent technique over provisional single stenting in true LM bifurcations (level of evidence: B).
Two trials diverge in LM bifurcation lesions
Following DKCRUSH-V, the European Bifurcation Club Left Main (EBC MAIN) trial demonstrated diametrically opposing results when the single stent strategy produced better results with upfront two-stenting.
Published in the European Heart Journal3, EBC MAIN enrolled 467 patients to examine outcomes of a two-stent strategy versus a stepwise provisional stenting approach that allowed for a second stent under prespecified procedural conditions.
Findings from EBC MAIN could be risky if it stimulates interventionalists to pursue stepwise provisional single stent strategy for the majority of patients.
EBC MAIN found no significant difference regarding the primary composite endpoint of death, myocardial infarction (MI), and target-lesion revascularization (TLR) at 1-year between the PS arm and the upfront two-stent arm (PS 14.7% vs. two-stent 17.7%, HR 0.80 95% CI, 0.5-1.3). Analysis of individual endpoints also produced no significant difference with similar rates of stent thrombosis (PS 1.7% vs. two-stent 1.3%), according to principal investigator David Hildick-Smith, MD (Royal Sussex County Hospital, Brighton, England).
Ą°Because we found no fundamental difference between the two groups, itĄŊs not necessary to prejudge the issue and decide up front that you need two stents,Ąą Smith said at a separate session at COMPLEX PCI 2021 Virtual. Ą°You can take it step-by-step and we found - interestingly - that only one-fifth (22%) of the provisional group actually needed a second stent. To say that we need two stents upfront, thatĄŊs usually wrong because you quite possibly donĄŊt.Ąą
EBC MAIN had simpler, shorter lesions; MACE rates subject to bias and Type II error
However, Chen pointed out key differences in study population and design that undermine the strength of EBC MAINĄŊs conclusions for most complex left main bifurcation.
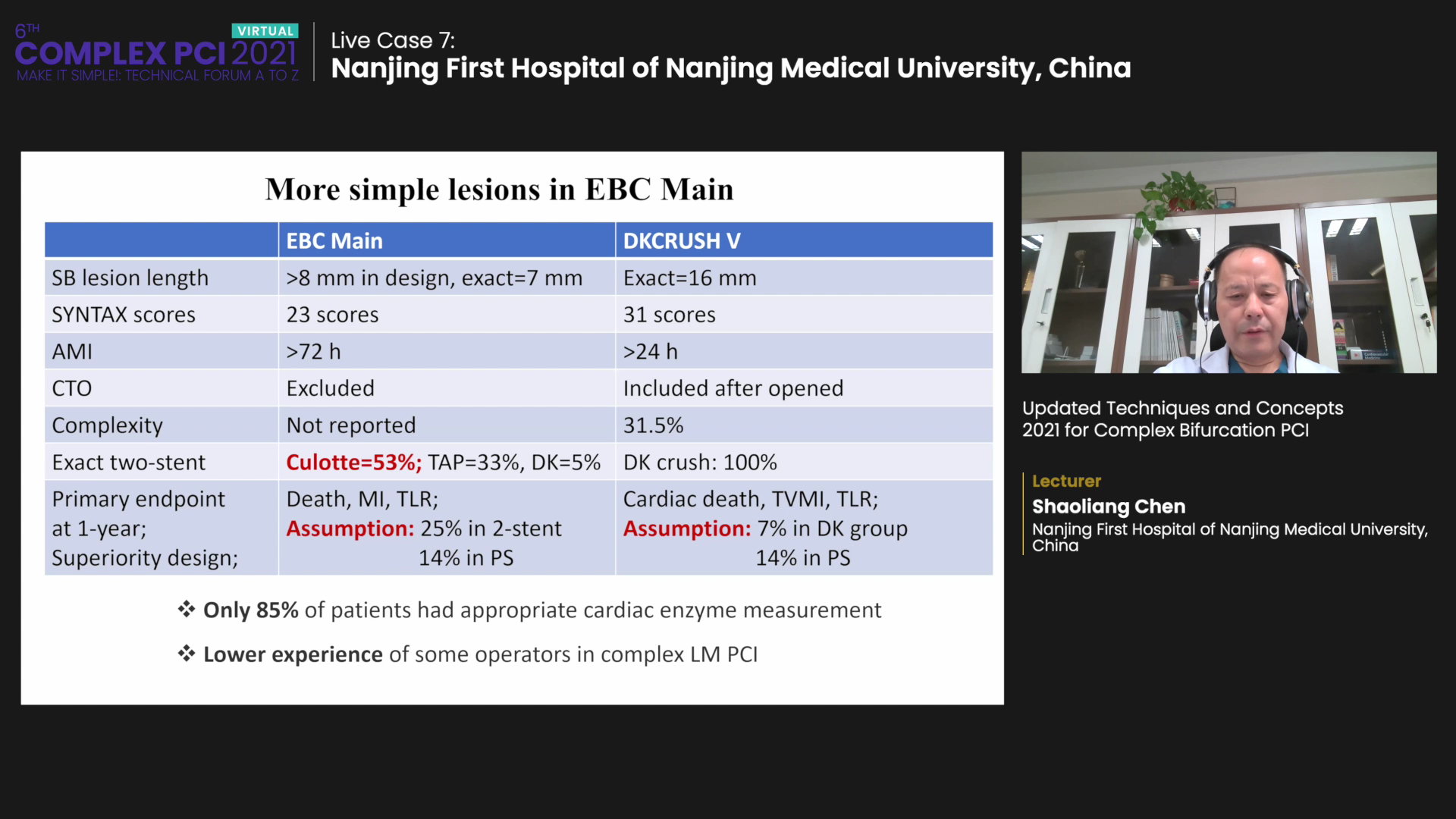
Foremost, EBC Main and DKCRUSH-V differed in the number of cases handled with the DK Crush technique in the upfront two stent arm: DK Crush was used in all patients in DKCRUSH-V but DK Crush accounted for only 5% in EBC MAIN and the majority was treated with Culotte (53%) or T and small protrusion (33%).
EBC MAIN also set the 1-year primary endpoint to death, MI and TLR. The assumed rates of primary endpoint occurrence were set to 25% in the double-stent arm and 14% in the PS arm, but outcomes resulted in 17.7% for the double-stent arm and 14.7% for the PS arm. Ą°This indicates that MACE rates were subject to bias and type II error,Ąą Chen said.
In contrast, DKCRUSH-V had set the 1-year primary endpoint to cardiac death, TVMI, and TLR. The assumed rate of primary outcome occurrence was 7% in the DK arm and 14% in the provisional stenting arm, with outcomes showing 10.7% versus 5.0% (p=0.02).
Ą°Both studies had a superiority design, but EBC MAIN showed neutral results, meaning it is a failed study,Ąą Chen said.
EBC MAIN also had patients with shorter side branch length (EBC MAIN >8 mm vs. DKCRUSH-V: 16 mm), lower SYNTAX scores (23 pts vs. 31 pts), more acute MI (>72 hours vs. >24 hours), and completed excluded chronic total occlusion (CTO) patients although DKCRUSH-V did not.
The overall higher death rates, MI, TLR, and stent thrombosis in EBC MAIN also indicate some operators had less experience with complex LM PCI. Chen noted that only 85% of patients in EBC MAIN had an appropriate enzyme measurement.
Considering longer side branches (ĄÃ10 mm) are associated with more negative outcomes of cardiac death, TVMI, TLR, TLF, and stent thrombosis, Chen highlighted the importance of differentiating between simple and complex bifurcation lesions and the length of the side branch according to DEFINITION criteria.
To address the ongoing debate, Chen said his team would conduct a study on LM bifurcation lesions (Medina 1,1,1 or 0,1,1) and enroll patients according to DEFINITION criteria to compare 1-year primary outcomes including TLF between provisional stenting and DK Crush.

