CASE20210828_003
Long and Heavily Calcified RCA Disease (From RCS to PLV Branch): Successful Image Guided Complex PCI
By
Presenter
Ashwani Sharma
Authors
1
Affiliation
, India1
Imaging - Invasive Imaging (IVUS, OCT, spectroscopy, etc)
Long and Heavily Calcified RCA Disease (From RCS to PLV Branch): Successful Image Guided Complex PCI
1
, India1
Clinical Information
Patient initials or Identifier Number
Mr. S P S
Relevant Clinical History and Physical Exam
This elderly gentleman had CAD-CCS ii symptoms in 2015. ECG had LBBB. EF was normal-was diagnosed to have single vessel disease in LCX (with small perfusion territory)- managed on GDMT. He had ACS in 2019 with LBBB rhythm and fall in ef to 40%. In cag apart from LCX, had tight and calcified RCA lesion- failed attempt of PCI due to calcium- was alright on GDMT. Now he had NSTEMI.


Relevant Test Results Prior to Catheterization
Creatinin was 1.48 (daibetes related CKD). EF was 40%. Normal sinus rhythm with LBBB was there in ECG as before.
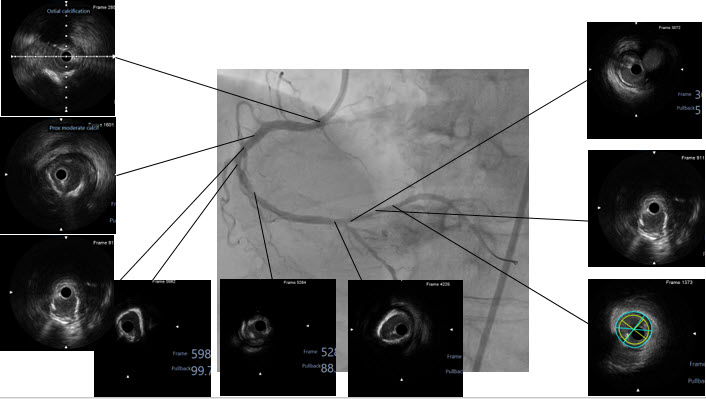
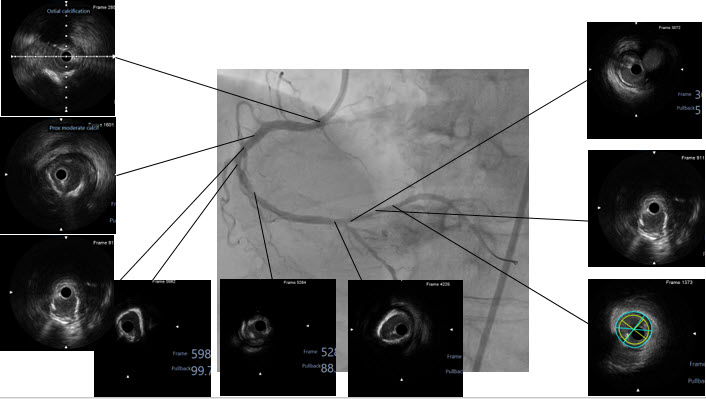
Relevant Catheterization Findings
RCA was normal. Noncritical plaques in lad while as before LCX had 80-90% stenosis. In RCA there was heavy calcium in ostio- proximal to distal. PDA proximal had tubular plaque-causing maximum 80-90% stenosis. Distal PDA had 95% stenosis.






Interventional Management
Procedural Step
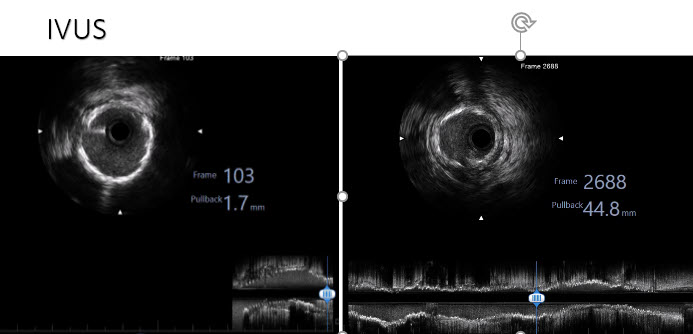
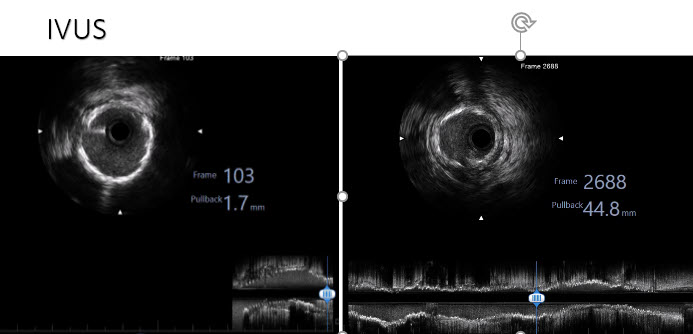
Through right transfemoral arterial access, 7 f jr guide was engaged to RCA (there was damping in pressure requiring recurrent disengagement). Through corsair micro-catheter sion wire was advanced in distal RCA but corsair could not be negotiated across the tightest lesion in mid-RCA (across RV branch). In parallel fashion rota, floppy wire was advance into PLV branch. Rota-ablation was performed with 1.5 mm burr. The PLV lesion was further pre dilated with semi compliant balloon of 2 mm diameter. IVUS was performed- 360 arc of calcium at multiple places seen. Further plaque modification was performed with 2.5 and 3.5 mm scoring balloon in PLV and whole RCA (the 2.5 mm ballon could only be advanced over grand slam wire with the help of guide extension catheter). Then 3 dess with adequate overlap were deployed form plv to ostial RCA (provisional cross over across PDA was opted as its ostium was free of disease). Adequate post dilatation was performed. IVUS guided in forthes podt dilatation in PLV to optimize the stent apposition. Good procedural and clinical outcome was achieved.






Case Summary
In this case, meticulous planning with all kind of cath lab hardware in guidance of intracoronary imaging led to the successful procedural and clinical outcome. Not to mention, team effort and patience was of course the root of success.
