CASE20240925_001
A Challenging Case Report: Coronary Atherectomy at Calcified In-Stent Restenosis Lesion
By Kyeongwon Seo
Presenter
Kyeongwon Seo
Authors
Kyeongwon Seo1
Affiliation
Asan Medical Center, Korea (Republic of)1,
View Study Report
CASE20240925_001
Complex PCI - In-Stent Restenosis
A Challenging Case Report: Coronary Atherectomy at Calcified In-Stent Restenosis Lesion
Kyeongwon Seo1
Asan Medical Center, Korea (Republic of)1,
Clinical Information
Relevant Clinical History and Physical Exam
The patient has a past medical history of PCI performed on July 30, 2001, at the proximal left anterior descending artery (pLAD). On July 16, 2006, the patient underwent a second PCI at the distal left circumflex artery (dLCX). The patient presented to our hospital on August 20, 2024, for regular follow-up after the procedure. The patient had no complaints at the time of the visit, and physical examination revealed no remarkable findings.
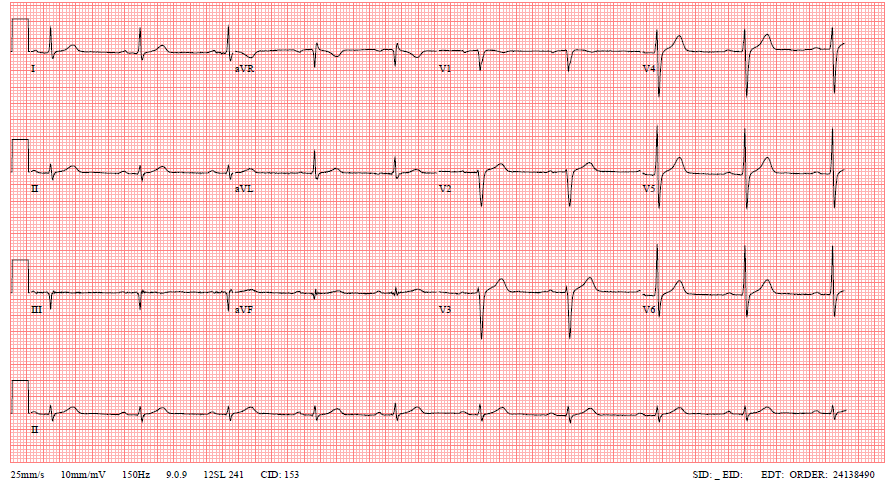
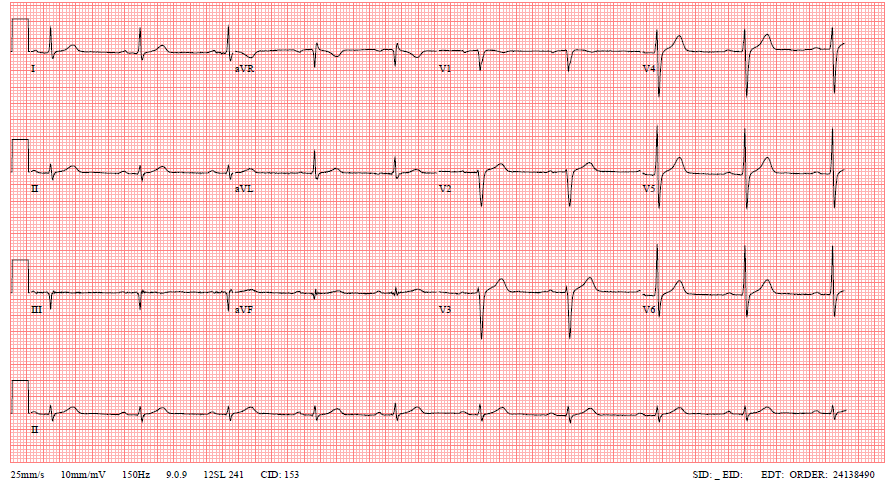
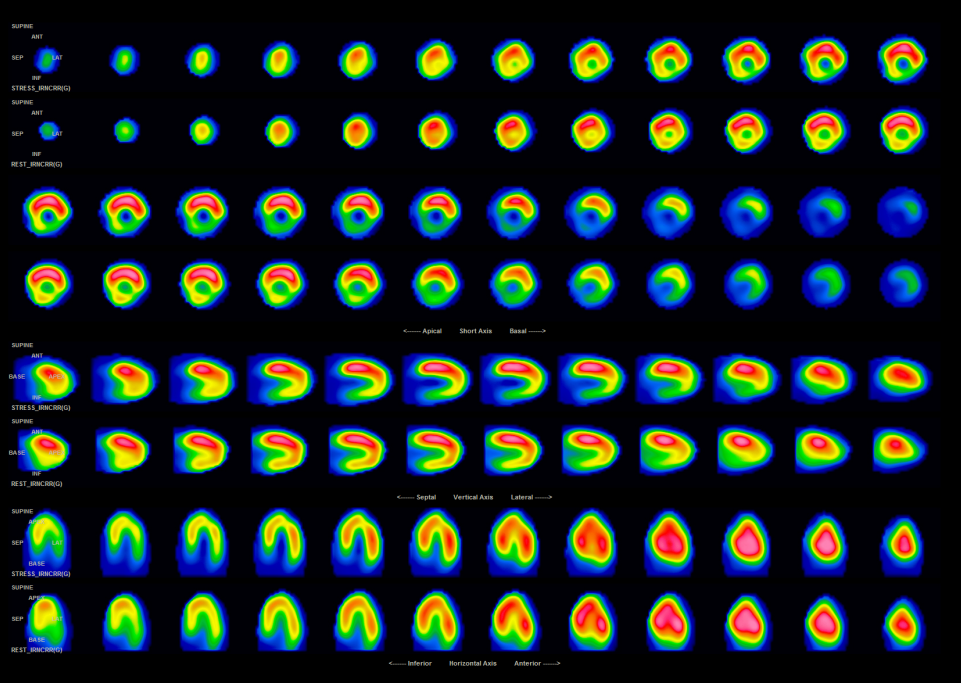
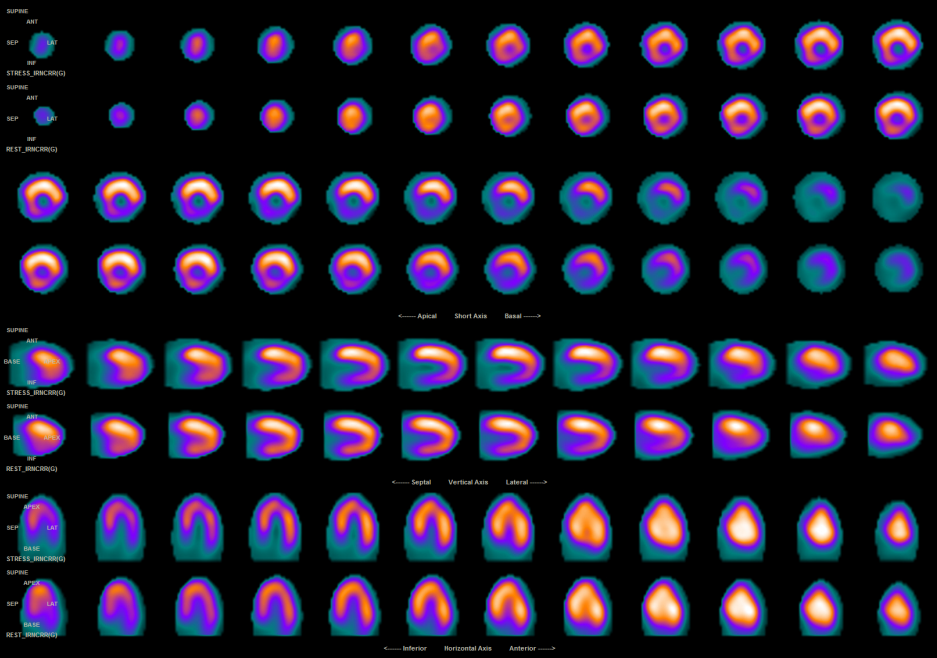
Relevant Test Results Prior to Catheterization
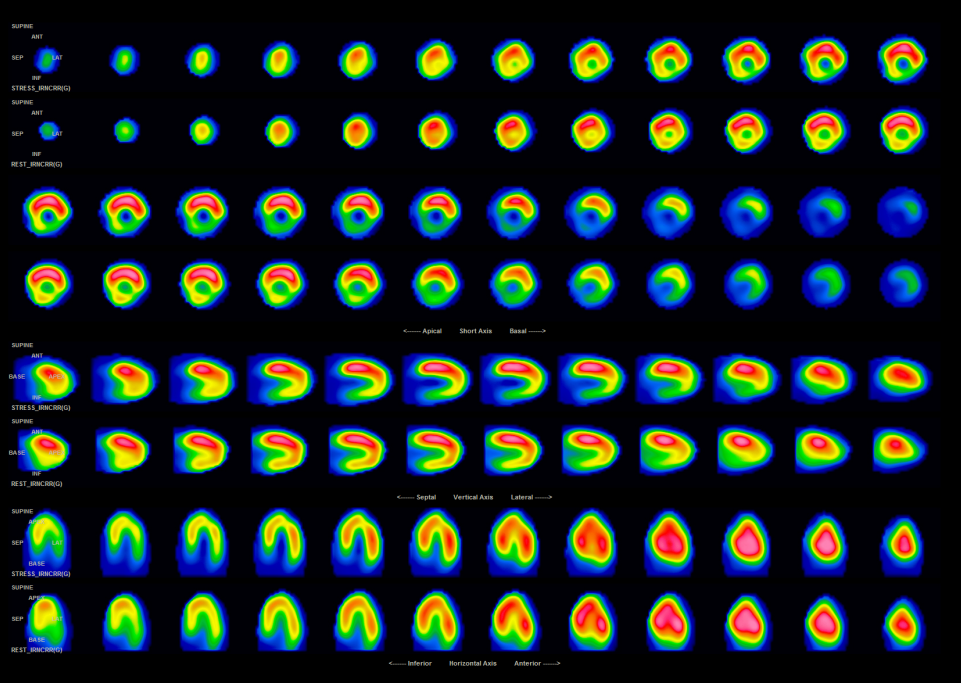
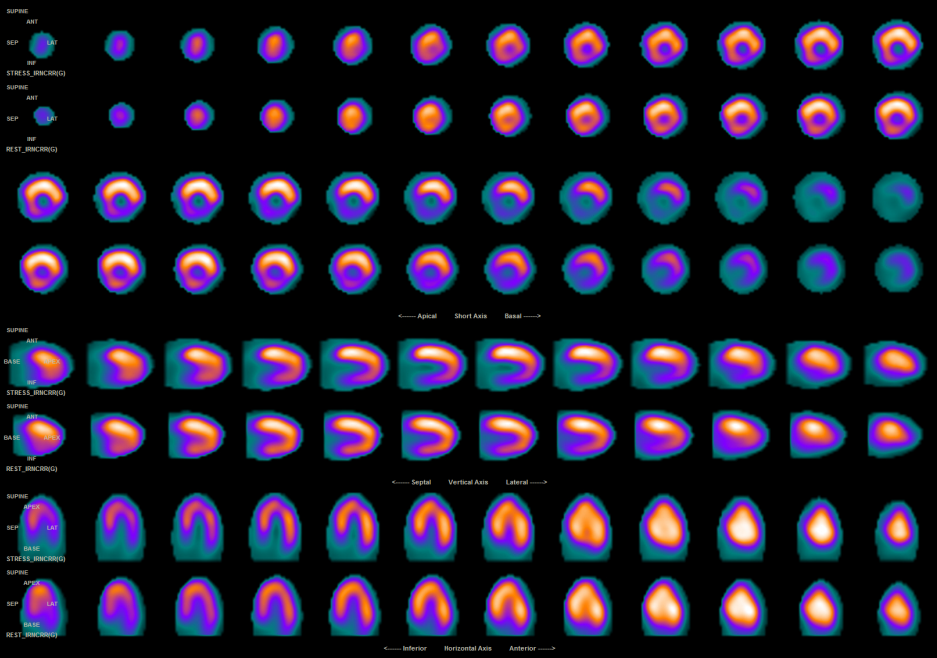
A myocardial SPECT performed for follow-up revealed a large reversible perfusion defect in the mid-basal inferolateral wall. As a result, coronary angiography (CAG) is planned.
Relevant Catheterization Findings
Coronary angiography (CAG) revealed that the stent in the proximal left circumflex artery (pLCX) was patent; however, in-stent restenosis (ISR) of the stent in the proximal mid left anterior descending artery (pmLAD) was identified. Therefore, percutaneous coronary intervention (PCI) is planned.
 이석한_CAG_LAD.avi
이석한_CAG_LAD.avi
 이석한_CAG_LCX.avi
이석한_CAG_LCX.avi
 이석한_CAG_RCA.avi
이석한_CAG_RCA.avi
Interventional Management
Procedural Step
The procedure was performed using an XB 6Fr guiding catheter. Intravascular ultrasound (IVUS) could not pass through the lesion in the proximal left anterior descending artery (pLAD), so predilatation was performed using a 2.5mm semi-compliant balloon and a 2.5mm non-compliant (NC) balloon. Afterward, a rotawire was advanced through the LAD using a Caravel microcatheter. Rotational atherectomy (rotablation) was then performed to address heavy calcification. Subsequently, post-dilatation was conducted with a 3.0mm NC balloon, and the procedure was completed by applying a 3.5mm drug-eluting balloon (DEB).
 이석한_PCI_ROTA.avi
이석한_PCI_ROTA.avi
 이석한_PCI_DEB.avi
이석한_PCI_DEB.avi
 이석한_PCI_final.avi
이석한_PCI_final.avi
Case Summary
Percutaneous coronary intervention (PCI) of severely calcified lesions is one of the most challenging procedures in interventional cardiology. Although calcified nodule (CN) within the stent has been reported as one of the causes of in-stent restenosis (ISR), the occurrence rate is relatively low, and the optimal therapy for these lesions is not clear. In patients with ISR accompanied by heavy calcification, rotational atherectomy can be an effective treatment option.
