CASE20240826_001
Precision Under Pressure: Navigating the Edge of Survival in Multivessel Coronary Artery Disease - A Case of ST-Elevation Myocardial Infarction with Cardiogenic Shock Needing a Hemodynamic Support Device in an Elderly Asian Female
By Phil Iver Guevarra
Presenter
Phil Iver Guevarra
Authors
Phil Iver Guevarra1
Affiliation
Chung-Ang University Gwangmyeong Hospital, Korea (Republic of)1,
View Study Report
CASE20240826_001
Complex PCI - Multi-Vessel Disease
Precision Under Pressure: Navigating the Edge of Survival in Multivessel Coronary Artery Disease - A Case of ST-Elevation Myocardial Infarction with Cardiogenic Shock Needing a Hemodynamic Support Device in an Elderly Asian Female
Phil Iver Guevarra1
Chung-Ang University Gwangmyeong Hospital, Korea (Republic of)1,
Clinical Information
Relevant Clinical History and Physical Exam
A 78-year-old female, known to be diabetic and dyslipidemic, presented with sudden onset of chest heaviness and dyspnea while working on her farm. This was associated with a dizziness and near syncope. Chest pain was graded 8/10, left parasternal area, non-radiating, heavy in character and not relieved with rest. On exam, she was tachycardic at 120 bpm, hypotensive at 80/60mmHg and tachypneic with RR of 24. On physical exam, neck veins were distended, crackles on chest auscultation.
 2.wmv
2.wmv
 3.wmv
3.wmv
Relevant Test Results Prior to Catheterization
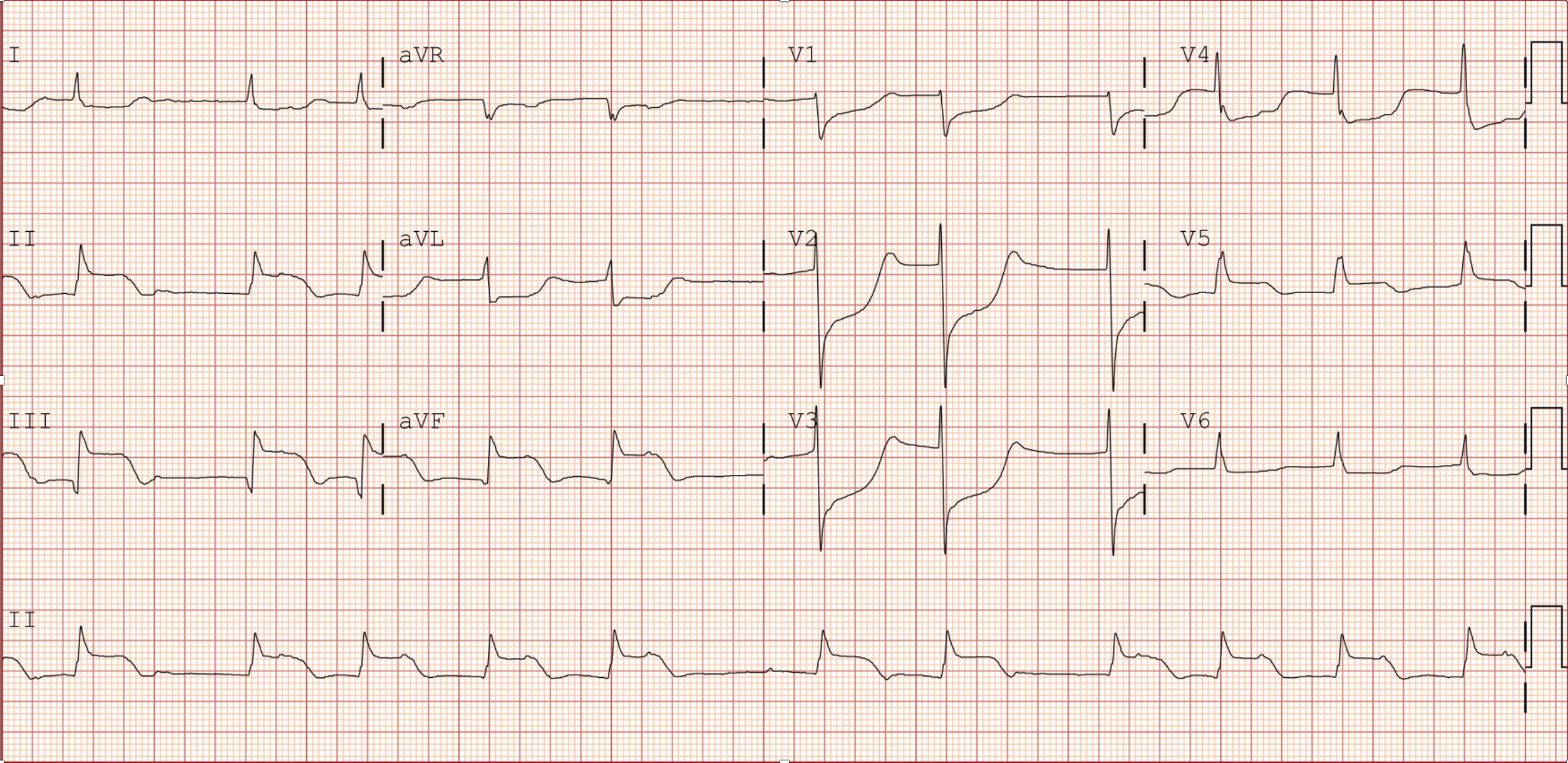
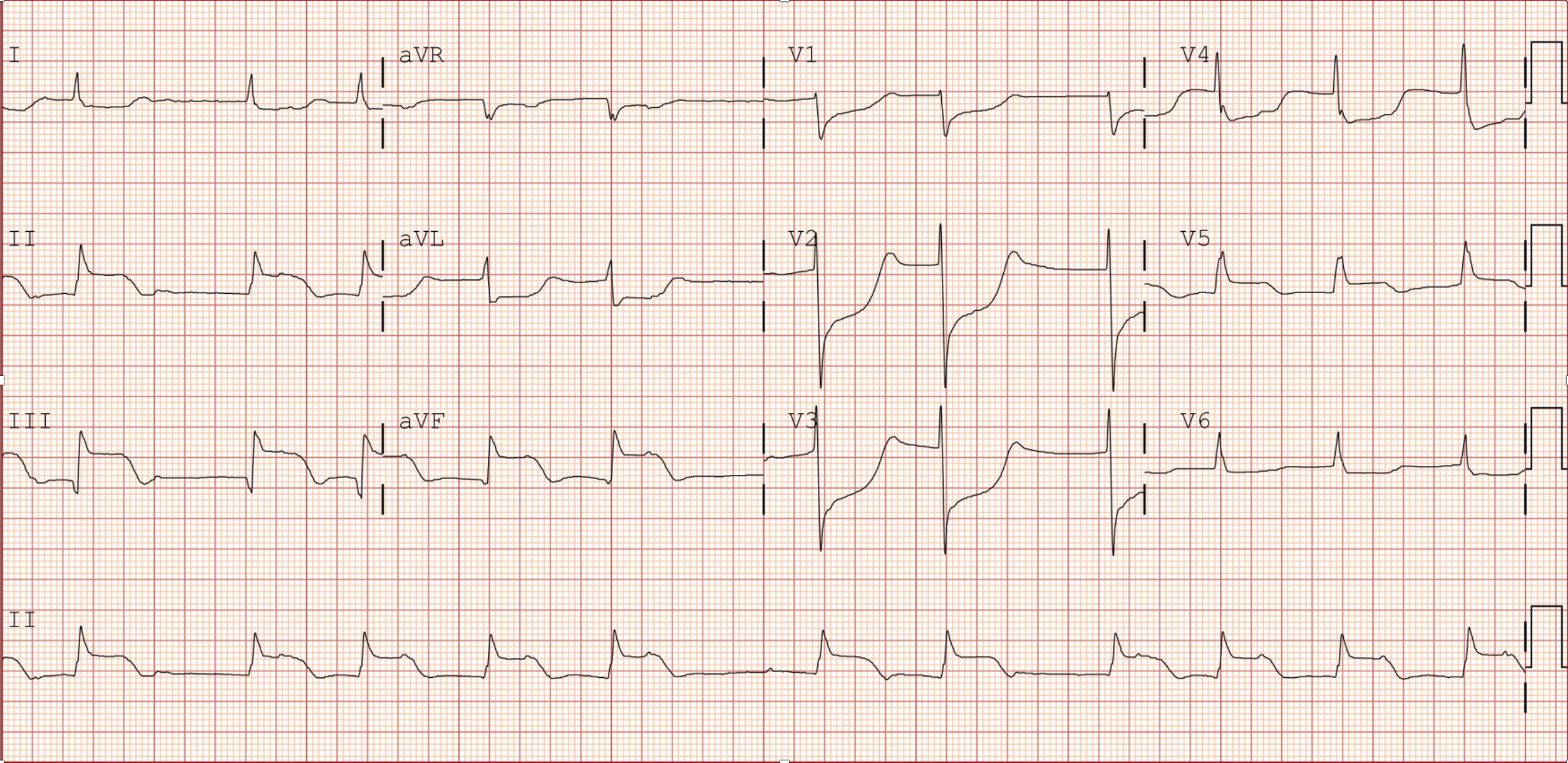
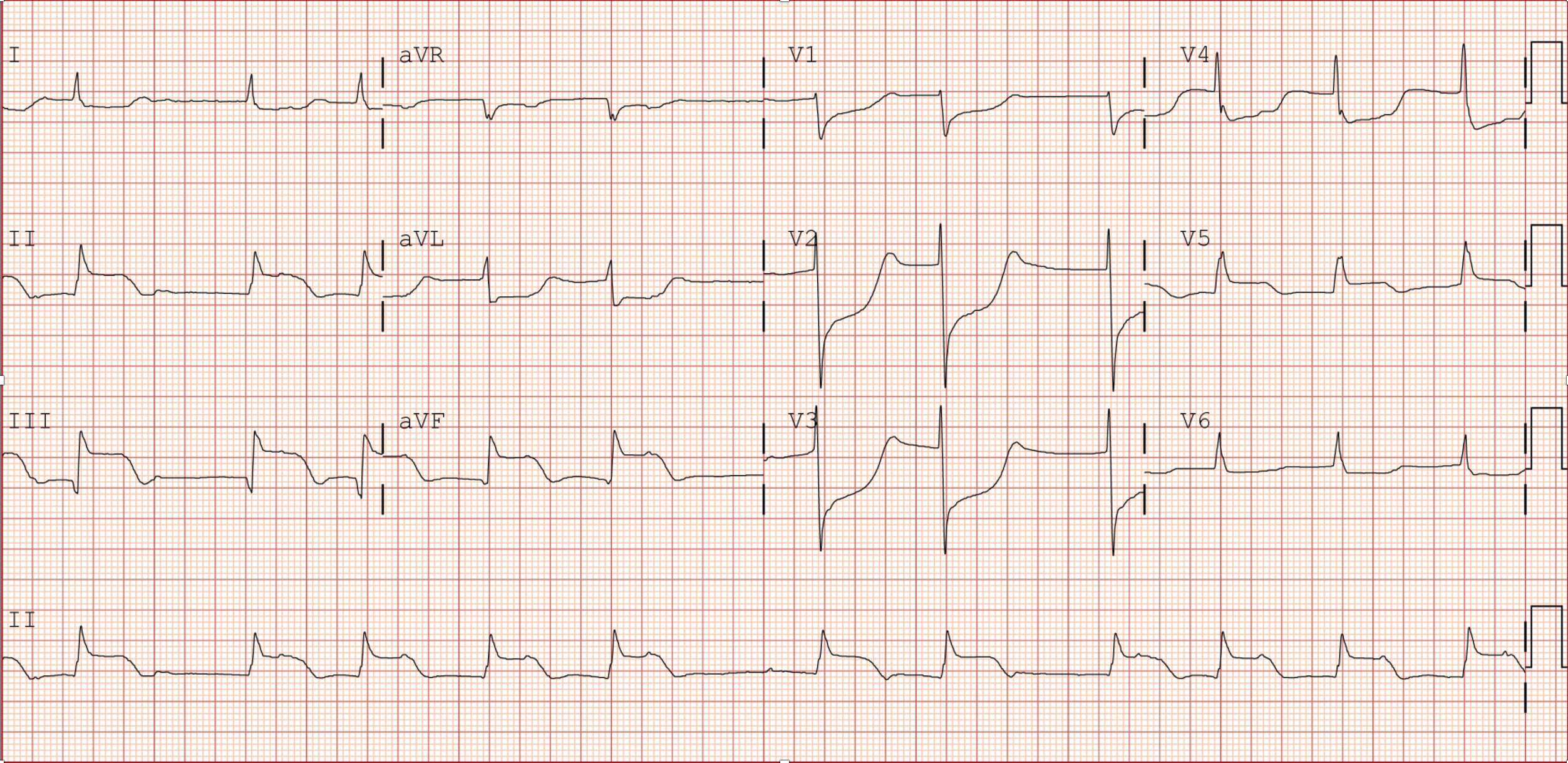
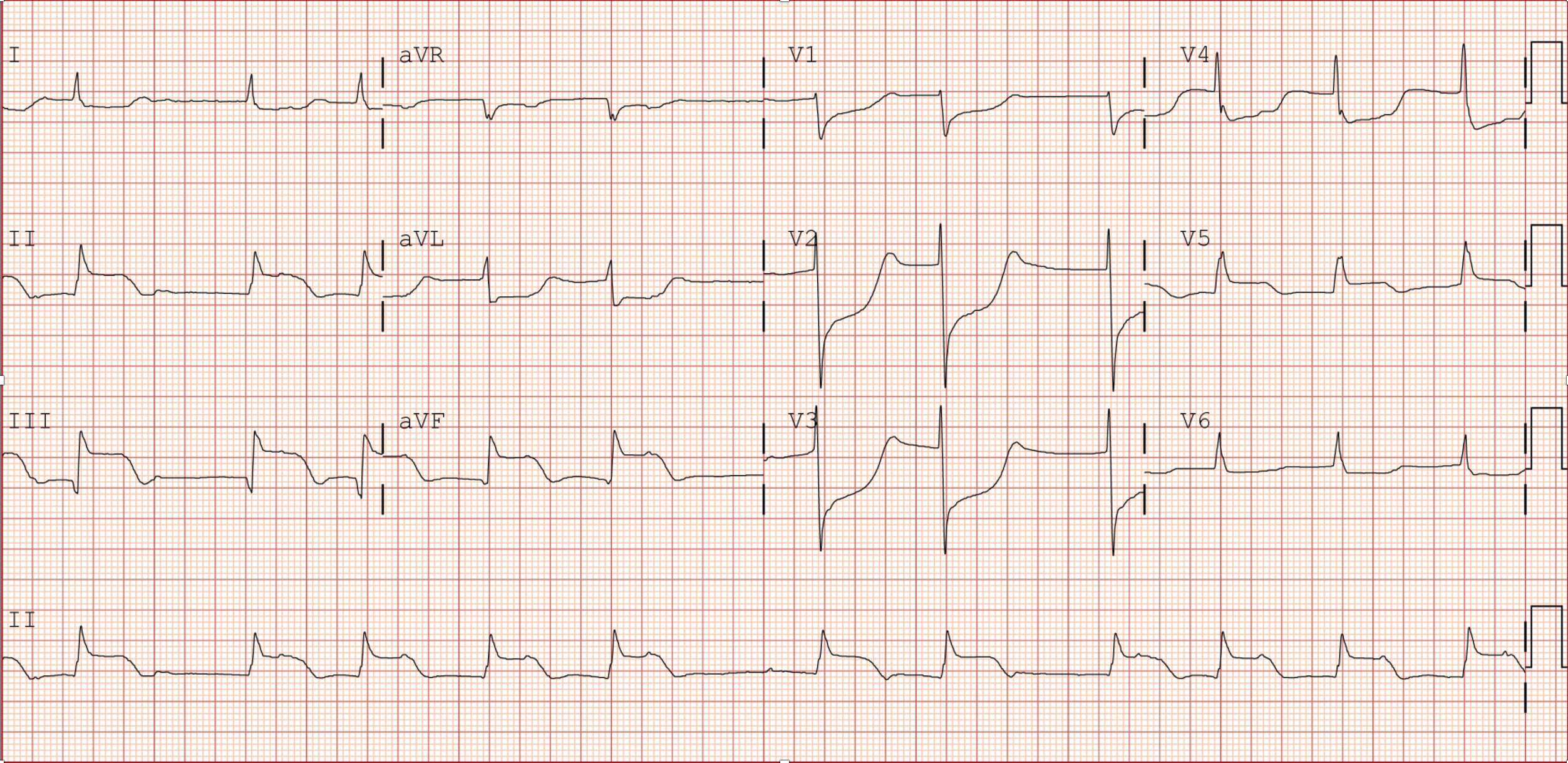
12-lead EKG showed ST-segment elevation in inferior leads, reciprocal changes, and complete heart block. Chest X-ray showed pleural effusion and pulmonary edema. Labs showed HS troponin I of 500,000 ng/L, NT-proBNP of 11,568 pg/mL, and an EF of 18.4% with akinesia in multiple walls on 2D echo.
 2.wmv
2.wmv
 3.wmv
3.wmv
Relevant Catheterization Findings
Severe three-vessel disease, specifically involving 70% stenosis of the distal left main (LM) segment, a bifurcation lesion with total occlusion of the proximal left anterior descending (LAD) artery and 80% stenosis of the proximal left circumflex (LCx) artery, and total occlusion of the distal right coronary artery (RCA).
Interventional Management
Procedural Step
Given the clinical presentation and initial findings, the distal RCA was identified as the culprit lesion, hence the decision to revascularize it first. The RCA was accessed with a JR 4.0, 6 French guide catheter and was wired with an Asahi Sion Blue guidewire. Balloon angioplasty was performed using an Ikazuchi 2.5 mm x 15 mm balloon at 16 atmospheres for 5 seconds. The stenosis was reduced to 50% from total occlusion, with no evidence of dissection or thrombus, and TIMI 3 flow was achieved. Despite the PCI and initial medical therapy, the patient remained persistently hypotensive. It was quickly decided to insert a temporary pacemaker, place the patient on venous-arterial extracorporeal membrane oxygenation (VA-ECMO) support, and perform complete revascularization once was more stable. After 2 days on VA-ECMO, the patient’s clinical status improved, and the second stage of revascularization was performed. IVUS-guided PCI of the left coronary arteries was initially done in the proximal to mid LAD with rotational atherectomy using a Rotablator 1.25 mm burr, followed by stenting from the LM to the mid LAD with Orsiro 3.0 mm x 40 mm and 2.5 mm x 26 mm stents, respectively. The LCx was successfully managed with a non-compliant balloon, and finally, the distal RCA revascularization was completed using an Orsiro 3.0 mm x 18 mm stent.
 lv_0_20240826190133.mp4
lv_0_20240826190133.mp4
 lv_0_20240826190248.mp4
lv_0_20240826190248.mp4
 lv_0_20240826190316.mp4
lv_0_20240826190316.mp4
Case Summary
After 10 days in the ICU, the patient's vitals improved. She was then weaned-off ECMO support. In total, she completed 19 days of hospitalization and was discharged stable with significant reduction of symptoms.
