CASE20240816_005
Unexpected Left Main Bifurcation Stenting in a Case of Multivessel PCI in ST-Elevation Myocardial Infarction
By Florimond Joseph Jr. Garcia
Presenter
Florimond Joseph Jr. Garcia
Authors
Florimond Joseph Jr. Garcia1
Affiliation
The Medical City, Philippines1,
View Study Report
CASE20240816_005
Complex PCI - Bifurcation
Unexpected Left Main Bifurcation Stenting in a Case of Multivessel PCI in ST-Elevation Myocardial Infarction
Florimond Joseph Jr. Garcia1
The Medical City, Philippines1,
Clinical Information
Relevant Clinical History and Physical Exam
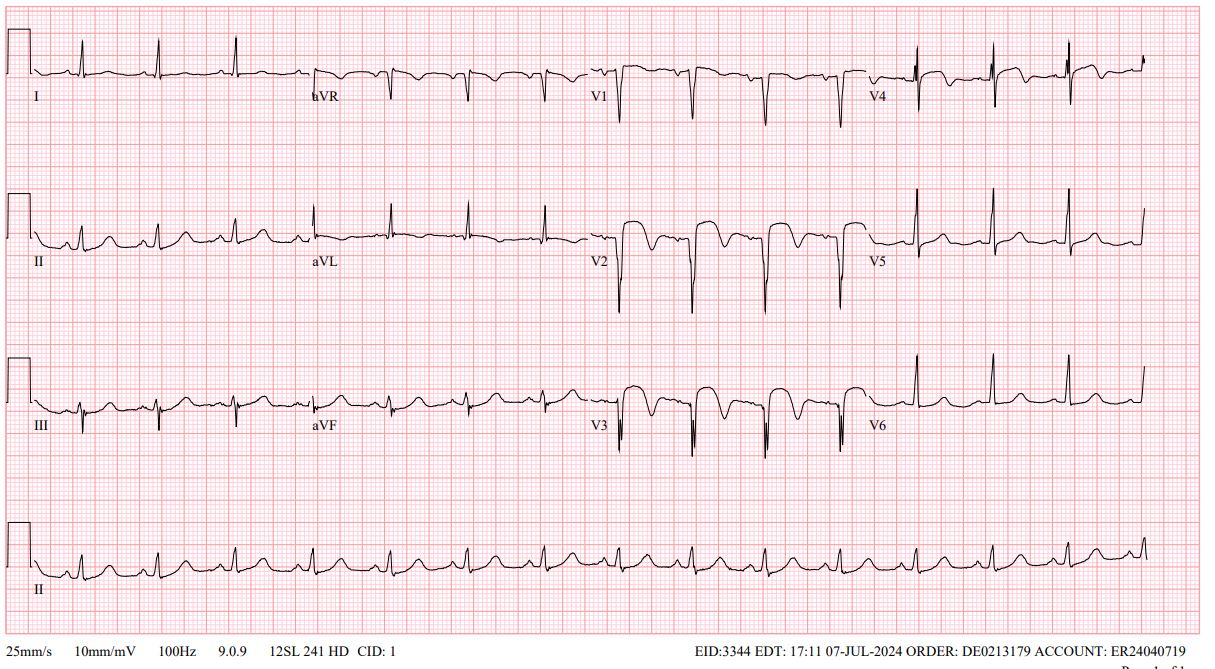
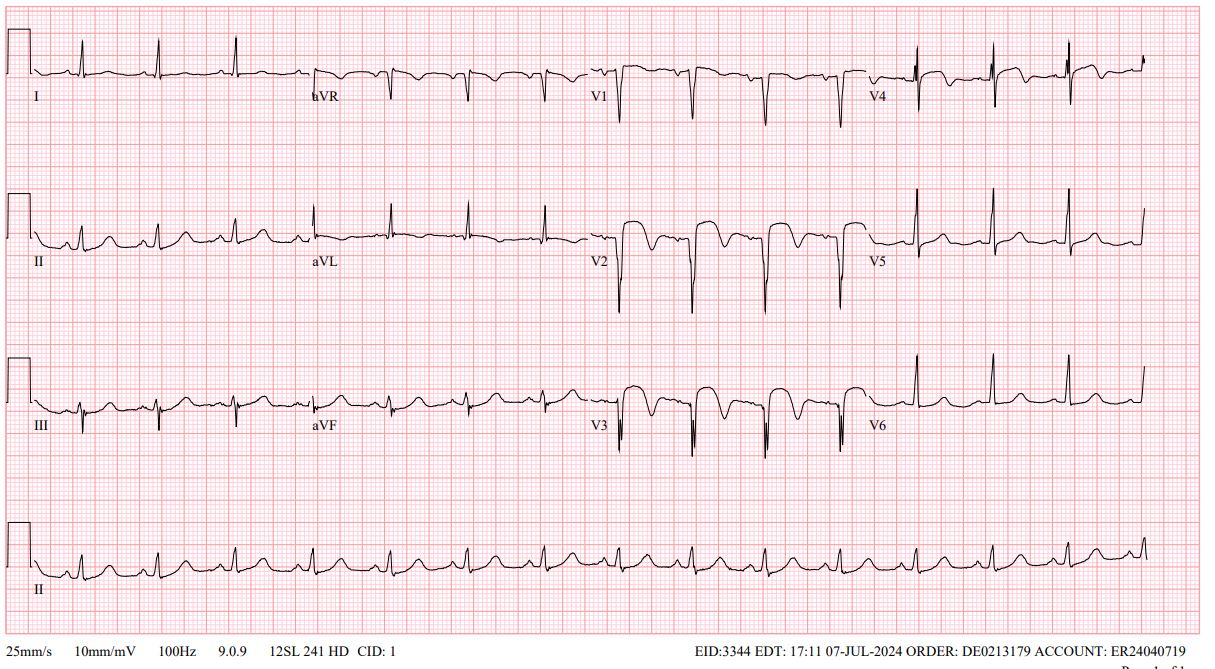
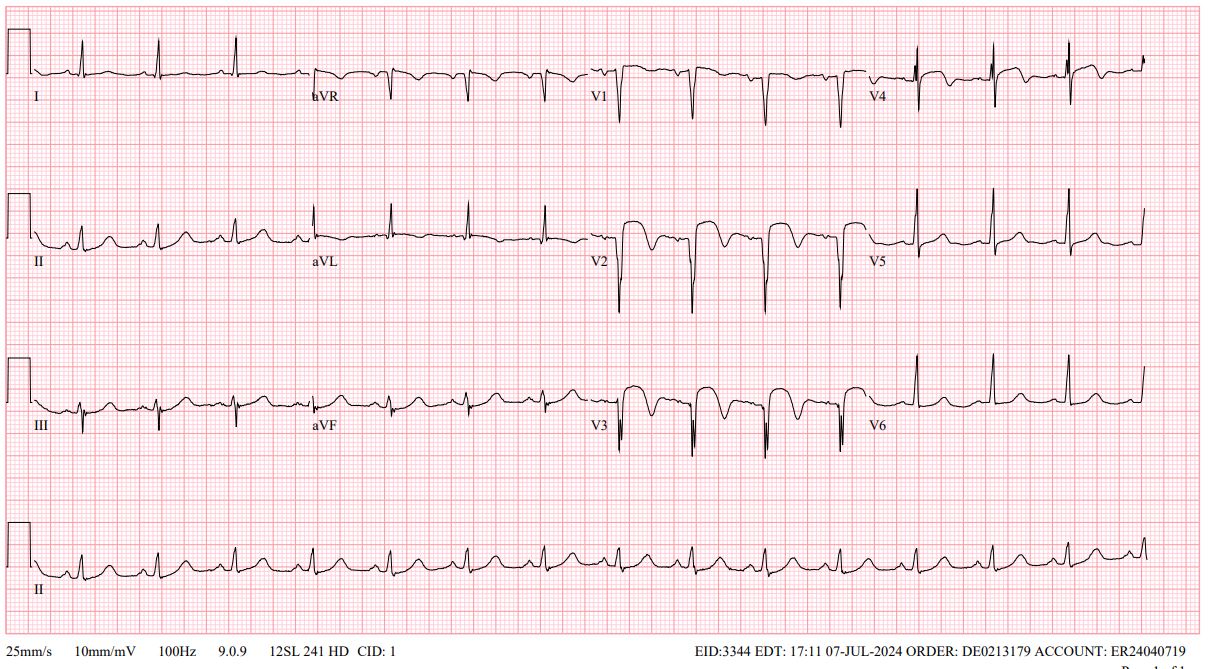
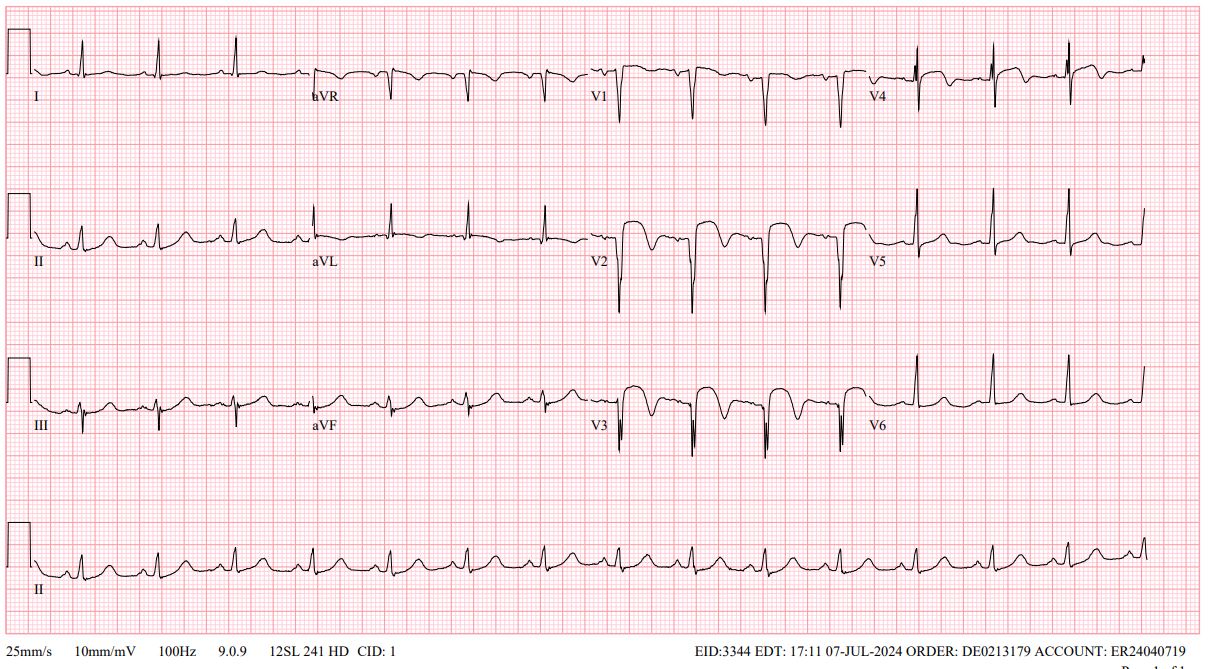
We are presented with a case of a 55 year old male, diabetic who came in due to sudden onset severe chest pain. 1 day prior to admission, the patient had sudden severe chest pain and was brought to a local hospital in a different country while the patient was on vacation. Allegedly, 12L ECG at the local hospital was anterior ST-Elevation and was advised for admission. However, the patient refused and flew back to the Philippines for emergency consult.
Relevant Test Results Prior to Catheterization
On arrival at the emergency room, 12L ECG done showed anterior wall ST-Elevation. POCUS 2D echocardiogram showed multi-segmental wall motion abnormality with reduced ejection fraction.
 Combined Clip.mp4
Combined Clip.mp4
Relevant Catheterization Findings
The LM is a large sized vessel with LI and it trifurcates into the LAD, RI and LCX. The LAD is a good sized, diffusely diseased type III vessel with an 80% ostio-proximal stenosis, and 80% mid segment stenosis. The LCX is a good sized, non-dominant vessel with a bifurcating MEDINA 1,1,1 stenosis at the level of the major obtuse marginal branch. The RCA is a large sized dominant vessel with an 80% ostial stenosis. The RI is a fair sized vessel with an 80% ostio-proximal stenosis
 CA LEFT COMBINED.mp4
CA LEFT COMBINED.mp4
 CA RIGHT.mp4
CA RIGHT.mp4
Interventional Management
Procedural Step
PCI with stenting of the culprit LAD was initially performed as the patient was in shock and with persistent chest pain. Pre-dilation was done with a 2.0mm x 20 mm PTCA catheter at the ostial LAD up to the midsegment. A 2.5mm x 28 mm stent was deployed at the mid LAD, followed by a DCB to the ostial first diagonal branch. A 2.75mm x 33 mm stent was then placed at the proximal to mid LAD overlapping the first stent. Then, a 3.0 mm x 12 mm stent was deployed at the ostial LAD. This resulted in stabilization of blood pressure and decrease in the chest pain of the patient. However, the proximal stent struts of the ostial LAD stent jailed the LCX and RI. Trial of rewiring was done but failed. Prolonged fluoroscopy time and increased dye usage resulted in the team deciding for a staged PCI for the remaining non-culprit vessels. After 4 days, the patient underwent completion PCI of the LCX and RCA. The team decided to do a left main Culotte bifurcation stenting technique despite an absence of a lesion at the ostial LCX due to the difficulty in rewiring the LCX and as the proximal stent struts of the LAD stent causing future complications and becoming a nidus for thrombus formation. With persistent trial of crossing the LCX with a wire, the team was able to cross it through the stent struts of the LAD and completion PCI was performed on the mid LCX and bifurcation stenting of the left main artery. The team then proceeded successful
 CA PRE BIFURCATION STENTING.mp4
CA PRE BIFURCATION STENTING.mp4
 LM BIFURCATION.mp4
LM BIFURCATION.mp4
 LM BIFURCATION FINAL.mp4
LM BIFURCATION FINAL.mp4
Case Summary
Culprit only versus complete PCI strategy should be done meticulously with consideration of the patient’s current state, maximizing imaging tools such as IVUS, and exploring different techniques in percutaneous coronary intervention. The team should always be prepared for possible complications of procedures despite their rarity. A heart team approach is best when there are dilemmas in the therapeutic strategies to be applied. The TEAM has successfully revascularized the patient, managed immediately post procedure and followed up after discharge.
