CASE20240814_002
Patient-tailored Management of Pregnancy-associated Myocardial Infarction: Providing Best Decision in Dilemma
By Novita Setiawan Lim, Pintoko Tedjokusumo, Aninka Saboe
Presenter
Novita Setiawan Lim
Authors
Novita Setiawan Lim1, Pintoko Tedjokusumo1, Aninka Saboe2
Affiliation
Bandung Advent Hospital, Indonesia1, Hasan Sadikin Bandung General Hospital, Indonesia2,
View Study Report
CASE20240814_002
ACS/AMI - ACS/AMI
Patient-tailored Management of Pregnancy-associated Myocardial Infarction: Providing Best Decision in Dilemma
Novita Setiawan Lim1, Pintoko Tedjokusumo1, Aninka Saboe2
Bandung Advent Hospital, Indonesia1, Hasan Sadikin Bandung General Hospital, Indonesia2,
Clinical Information
Relevant Clinical History and Physical Exam
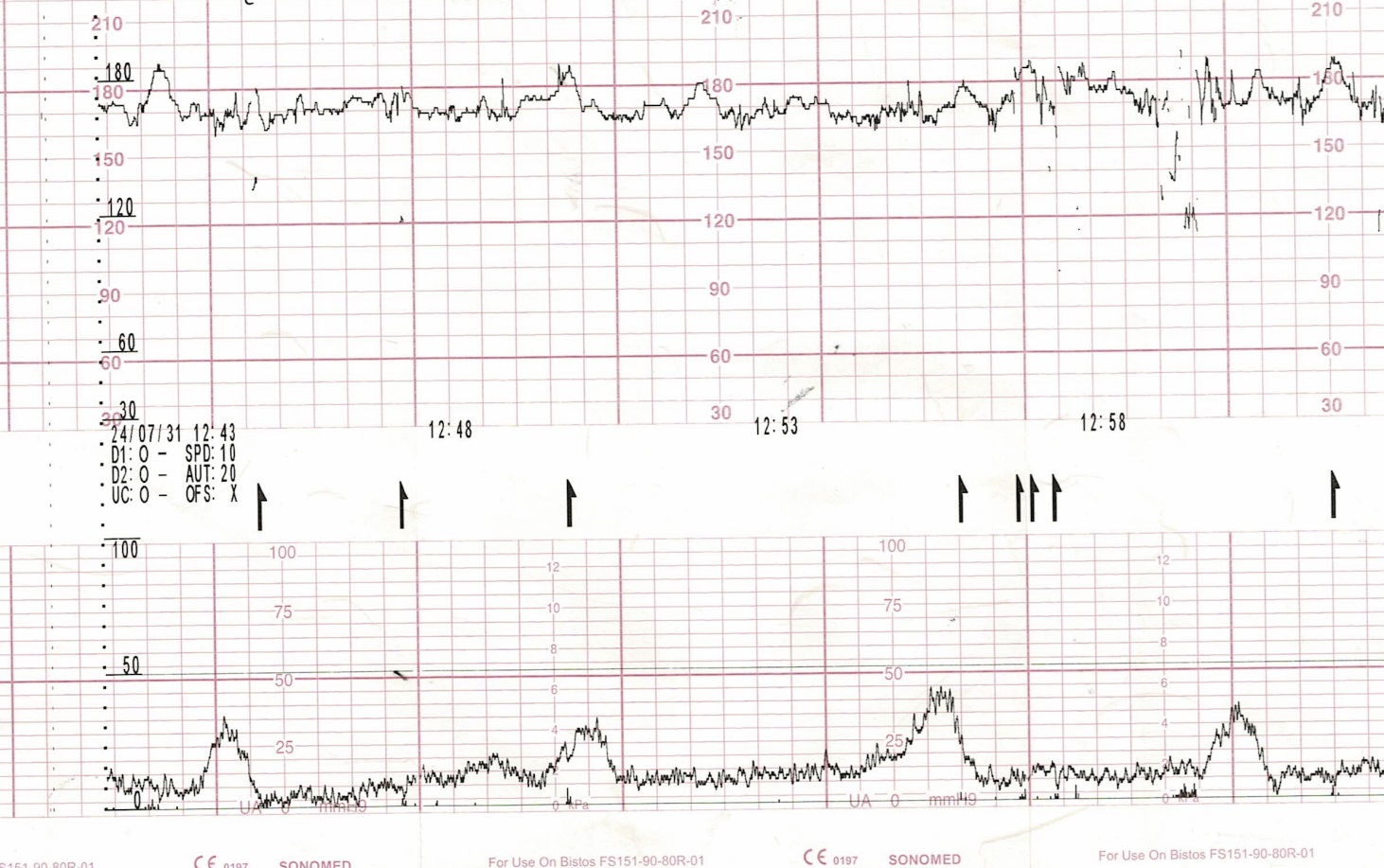
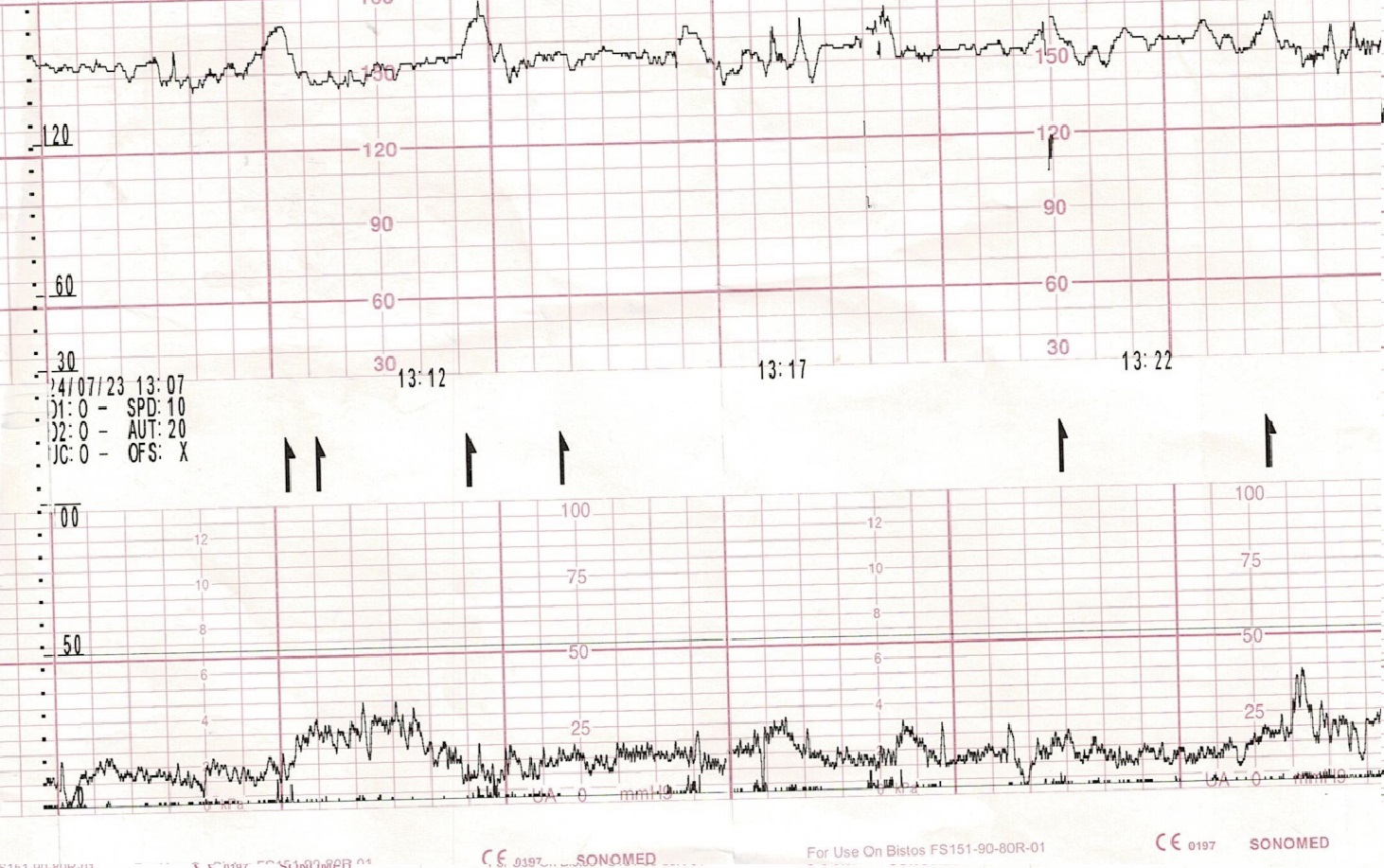
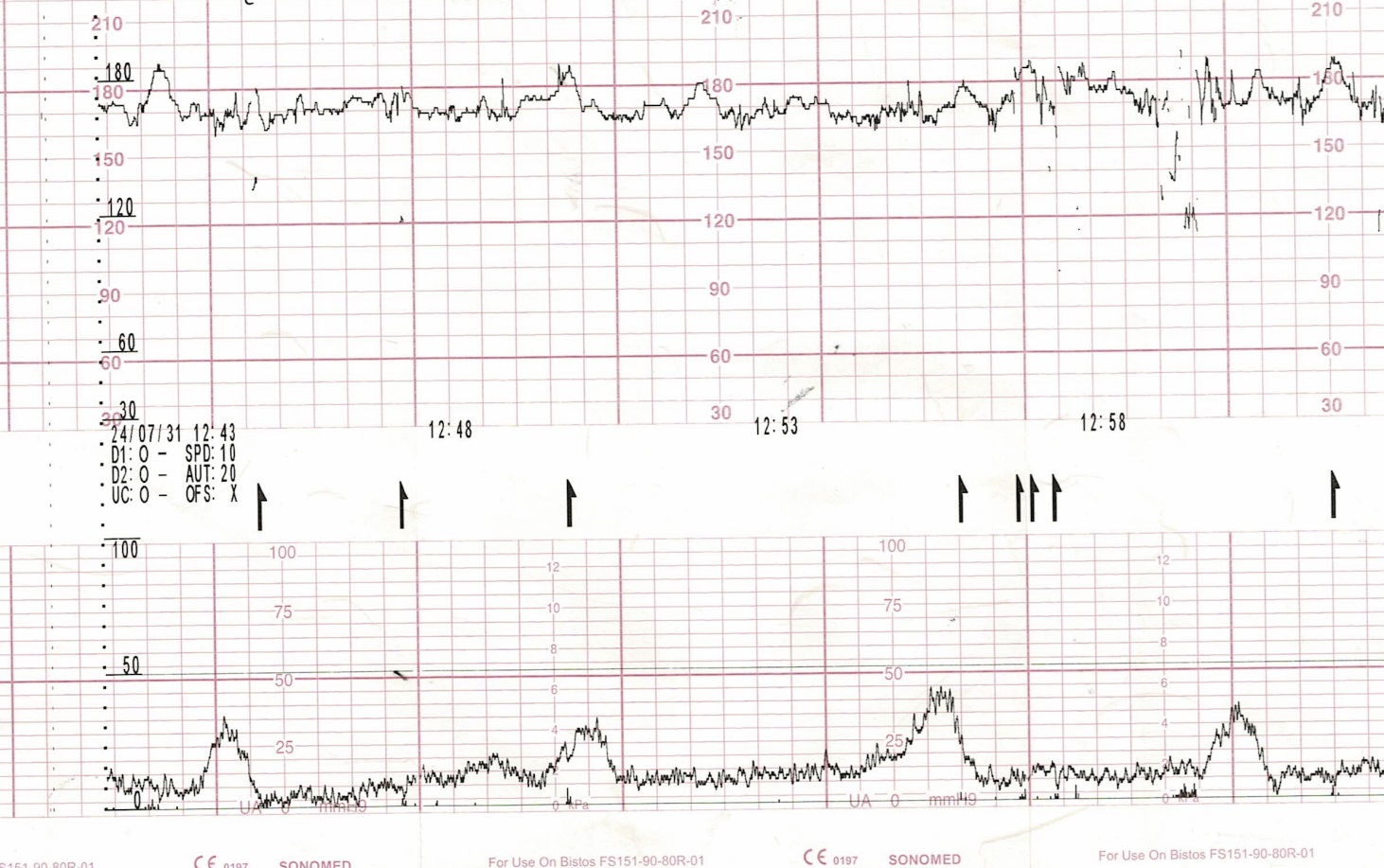
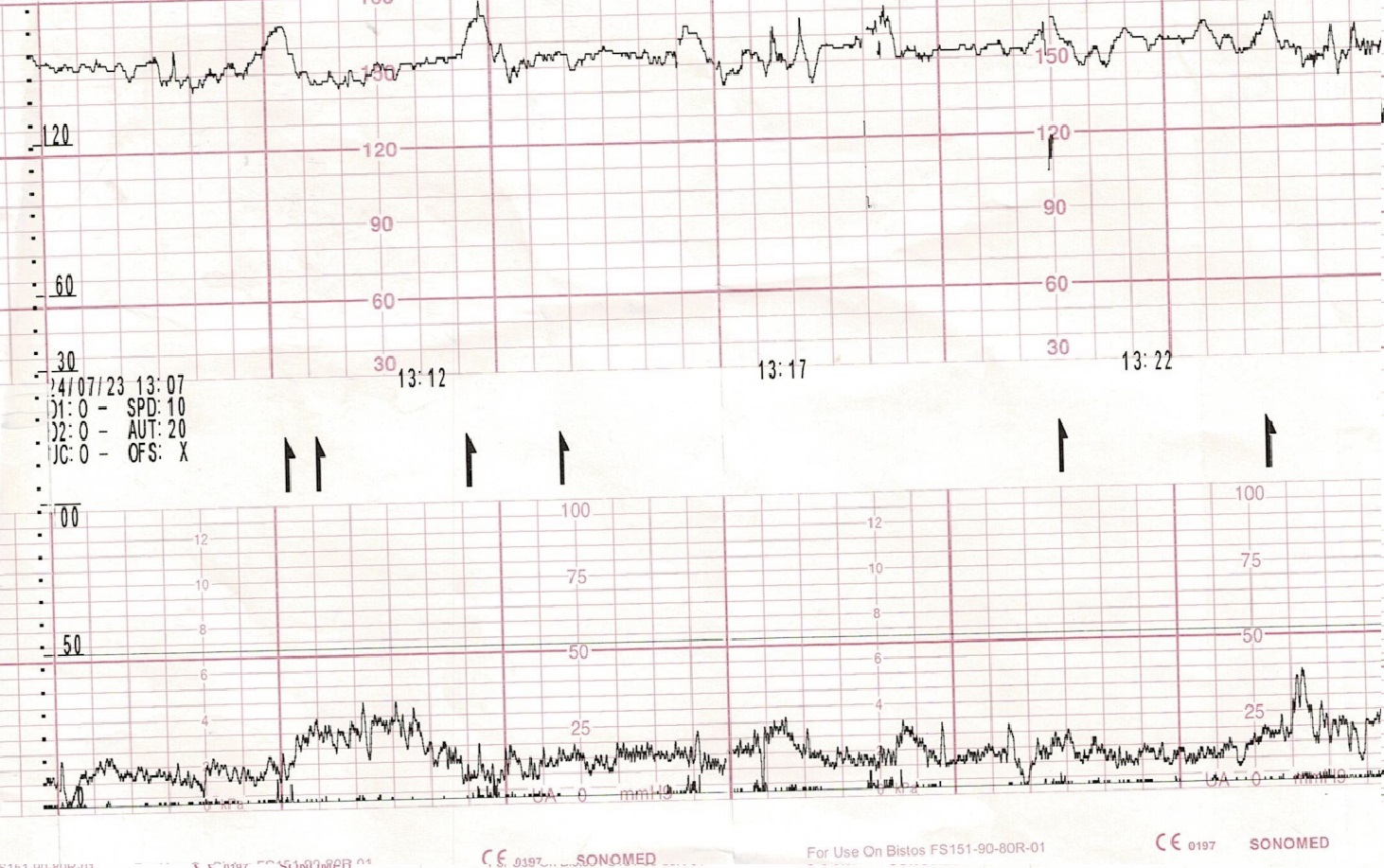
We report 2 cases of pregnancy-associated myocardial infarction (PAMI). The first case was a female, 36 years old, G9P4A5 without cardiovascular risk factor, came to emergency department at 24th week of pregnancy due to severe chest pain. The second case was a female, 42 years old, G2P2A0 with diabetes mellitus type 2, came at 18th week of pregnancy due to chest pain. In both cases, patients had unremarkable first trimester of pregnancies, both patients and fetal conditions were stable.
Relevant Test Results Prior to Catheterization
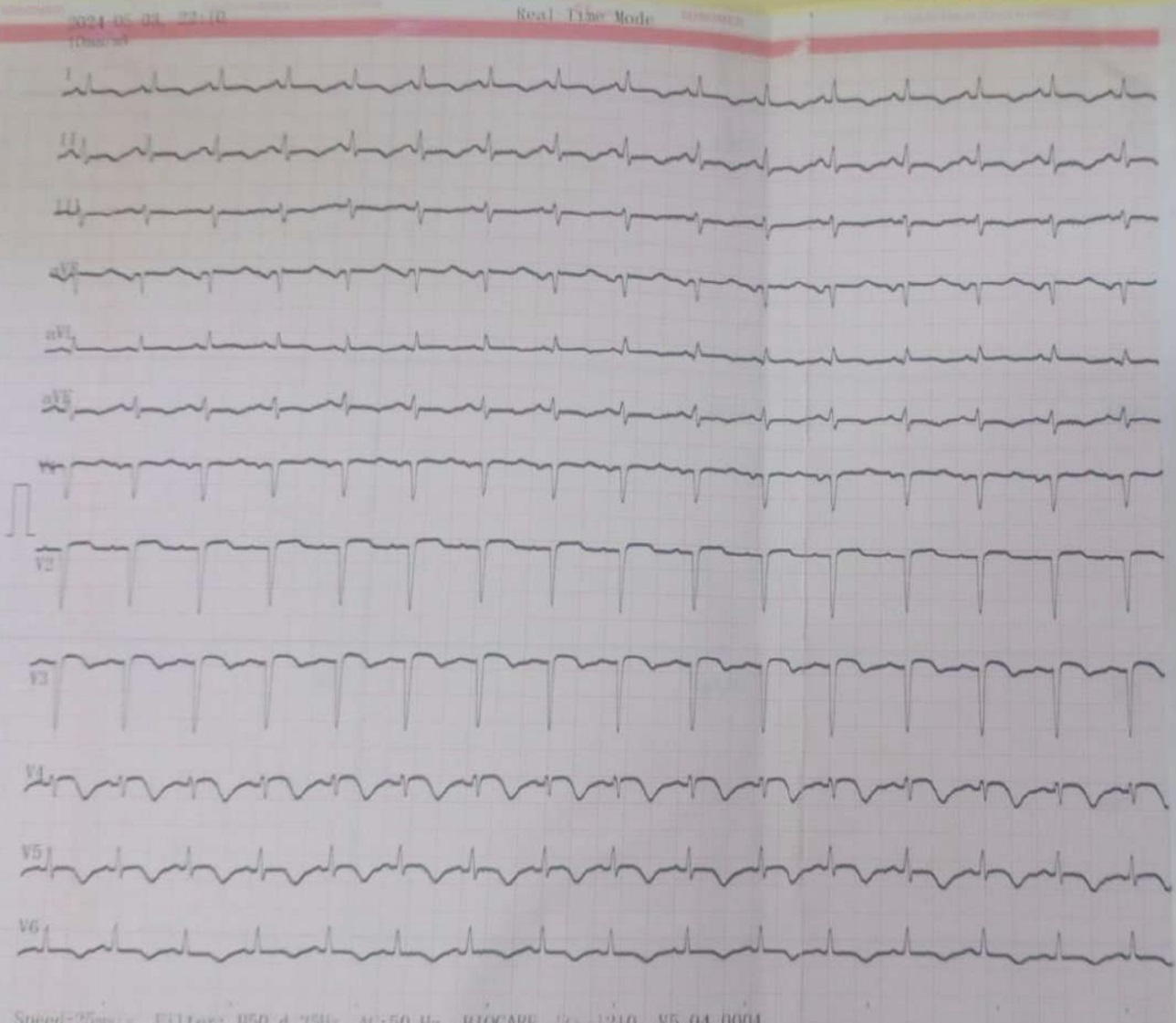
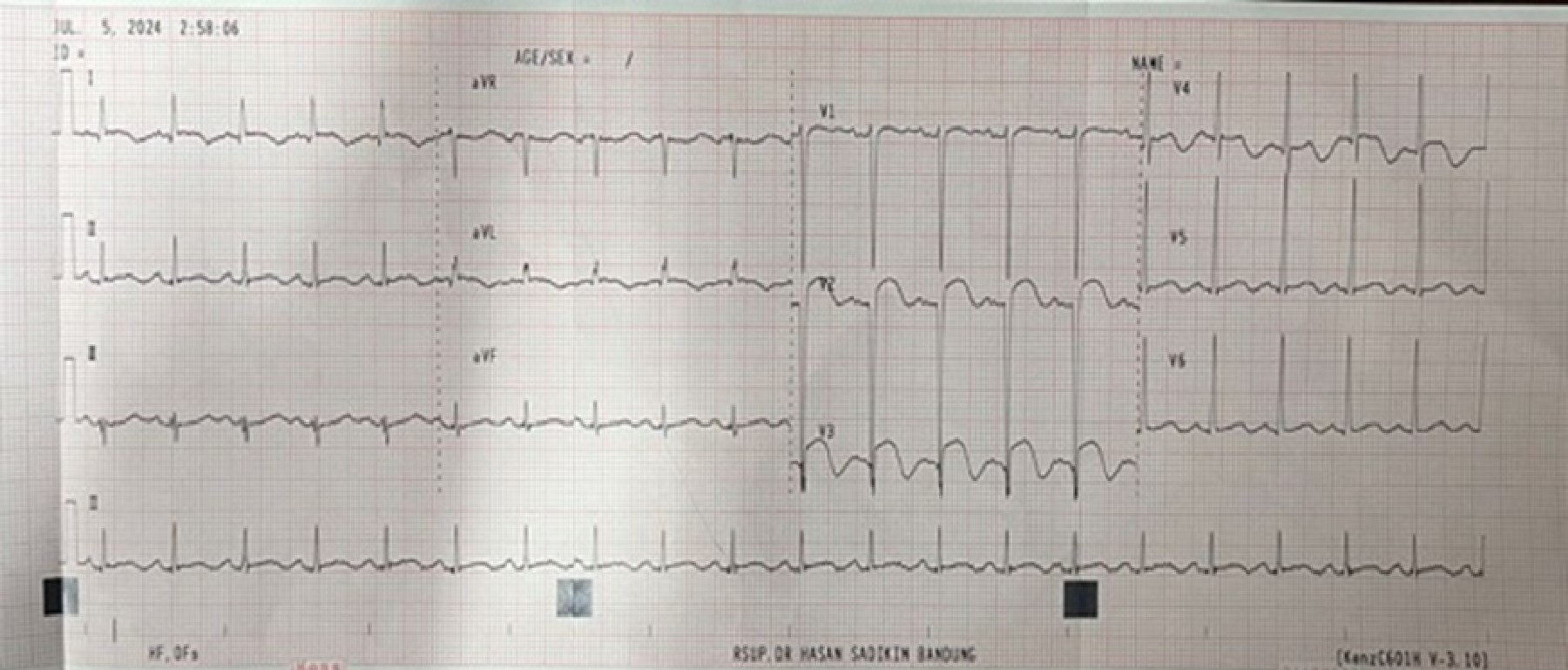
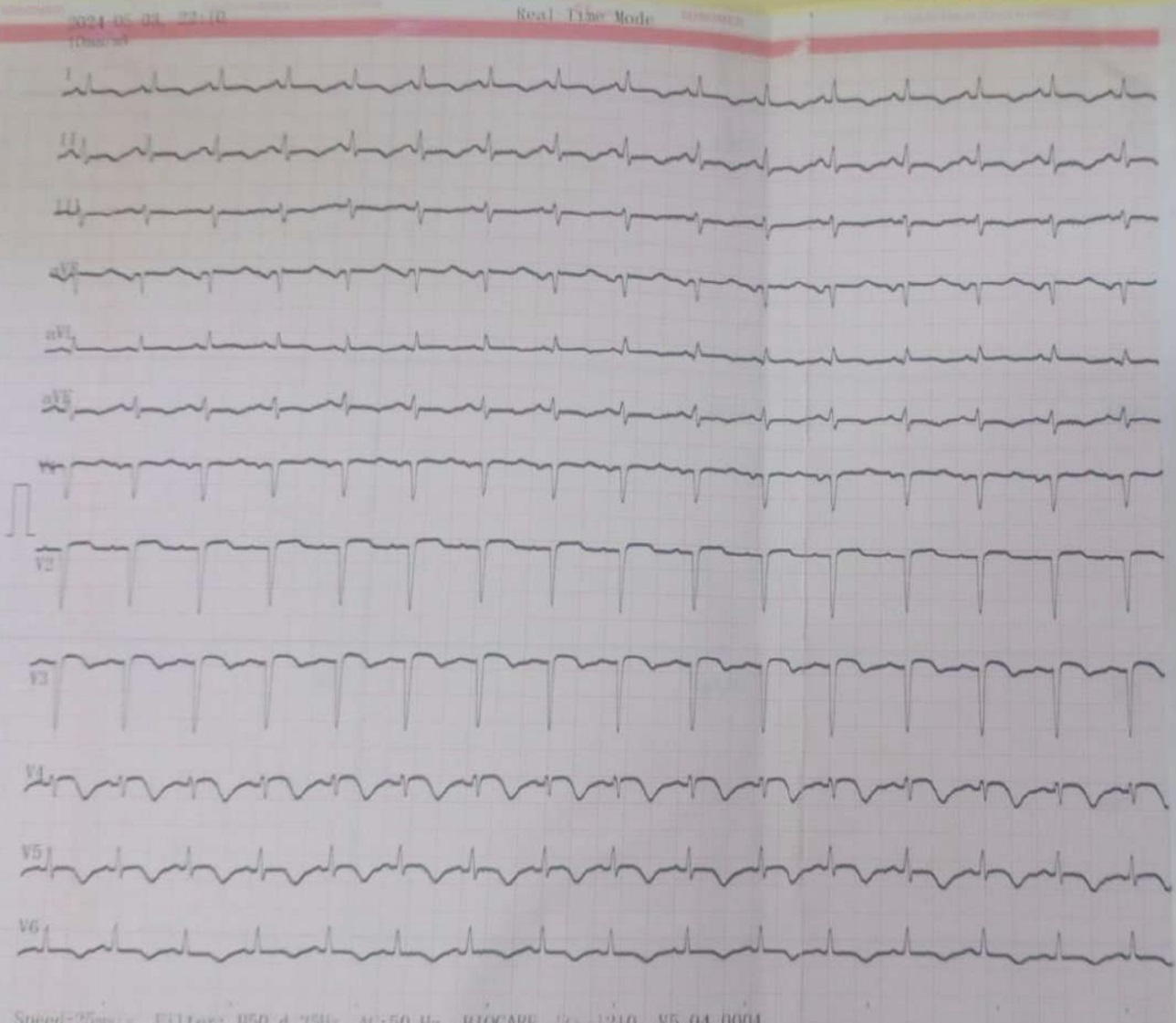
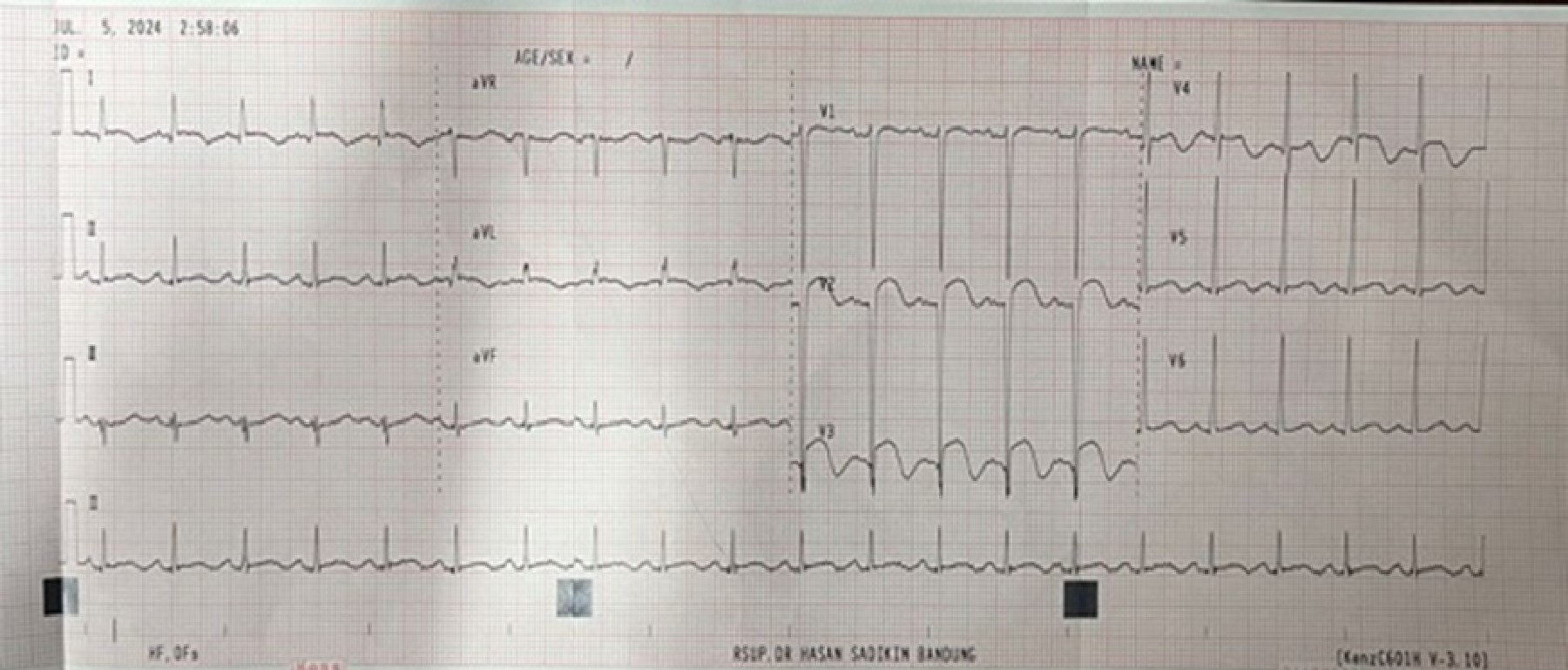
Both ECGs showed anteroseptal MI. Trans thoracal echocardiography in first and second cases showed normal left ventricular (LV) dimension, decreased LV function (LVEF Biplane 40% in first case and 47% in second case) with regional wall motion abnormalities (hypokinetic mid anterior and anteroseptal wall in first case and hypokinetic mid-apical anterior in second case). Cardiac markers were elevated in both cases.
Relevant Catheterization Findings
Angiography of the first case showed co-dominant system with subtotal occlusion at proximal left anterior descending artery (LAD), meanwhile left main, left circumflex, and right coronary arteries were free of significant disease. Second case angiography showed right dominant system with mild stenosis, haziness and radiolucent appearance at mid LAD with TIMI 3 flow. Left main, left circumflex, and right coronary arteries were free of significant disease.
 Spider Case1.mp4
Spider Case1.mp4
 RAO Caudal Case1.mp4
RAO Caudal Case1.mp4
 LAO Cranial Case 2.mp4
LAO Cranial Case 2.mp4
Interventional Management
Procedural Step
Both procedures were performed using abdominal shield. First procedure was done via right brachial artery, using diagnostic catheter JL and JR 3.5 6 Fr and Iomeprol 350. Guiding catheter JL 3.5 6 Fr was used to cannulate the left coronary circulation and wire Pilot 50 was advanced until it traversed proximal LAD lesion. Angioplasty was performed using balloon 3.0 mm (up to 12 atm) and 3.5 mm (up to 10 atm), followed by deployment of a 3.5/24 mm drug-eluting stent (DES) (Biofreedom) at 8 atm. Post dilatation was performed using NC balloon 4.0 mm (up to 18 atm) with an excellent final angiographic result, chest pain resolved, and ECG ST segments returned to baseline. Procedure time was 32 minutes (7 minutes fluoroscopy, total radiation dose of 1.190 mGy), and 140 cc contrast was used. Patient received 300 mg oral aspirin, 600 mg oral clopidogrel and 8.000 IU intra-venous unfractionated heparin. The remainder in-patient recovery was uncomplicated and she was discharged with oral aspirin, prasugrel, and bisoprolol throughout pregnancy. The patient underwent caesarean section delivery at 38 weeks without bleeding or any other complications and the baby was born healthy. Second case was done via right radial artery, using diagnostic catheter Tiger 5Fr and Iohexol 350. Procedure time was 11.52 minutes (1.43 minutes of fluoroscopy, total radiation dose of 115 mGy), and 40 cc contrast was used. Patient was managed conservatively with oral aspirin and clopidogrel throughout pregnancy.
 Stenting Case1.mp4
Stenting Case1.mp4
 Postdilatation Case1.mp4
Postdilatation Case1.mp4
 Final Angiogram.mp4
Final Angiogram.mp4
Case Summary
Sudden chest pain in pregnancy can be caused by cardiac and non-cardiac causes. PAMI should be suspected in pregnant women presenting with cardiac arrest, acute onset angina, ischemic ECG changes, or elevated cardiac biomarkers. Revascularization should be done when there is an absolute indication and restricted only for patient with unstable condition or high-risk features, to ensure preservation of TIMI 3 flow. Meticulous maternal and fetal protection, drug-consideration, bleeding risk assessment, contrast dose, arterial access, stent selection, experienced operator, and multidisciplinary approach tailored to each patient is mandatory in managing PAMI to improve maternal and fetal outcomes.
