CASE20240809_005
A Challenging Early Invasive Strategy: Bail-out Stenting in the Event of Stent Loss
By Markz Sinurat, Rha Seung-woon
Presenter
Markz Sinurat
Authors
Markz Sinurat1, Rha Seung-woon1
Affiliation
Korea University Guro Hospital, Korea (Republic of)1,
View Study Report
CASE20240809_005
ACS/AMI - ACS/AMI
A Challenging Early Invasive Strategy: Bail-out Stenting in the Event of Stent Loss
Markz Sinurat1, Rha Seung-woon1
Korea University Guro Hospital, Korea (Republic of)1,
Clinical Information
Relevant Clinical History and Physical Exam
A 71-year-old male complained of exertional angina (NRS 5/10), 7 hours before admission. His vital signs were stable. He was referred from another hospital for coronary evaluation. Risk factors: hypertension, diabetes mellitus, and history of percutaneous coronary intervention (PCI, 2019) to Ramus. Six-month follow-up revealed moderate Type 2 in-stent restenosis (ISR, 60%). Current treatment: Aspirin 100 mg, Pitavastatin/Ezetimibe 2/10 mg, Carvedilol SR 8 mg, Losartan 50 mg, Trimetazidine MR 35 mg.


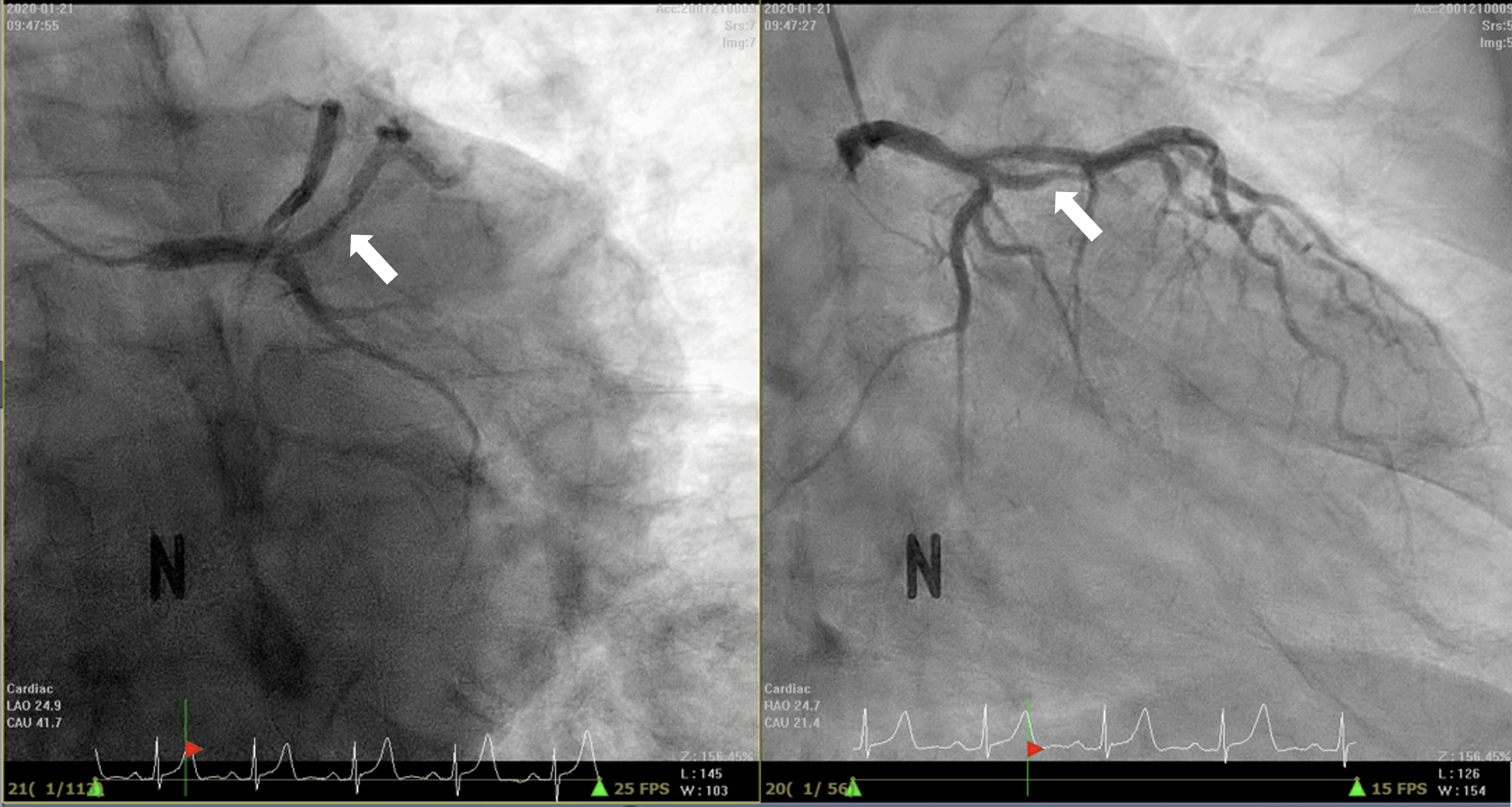
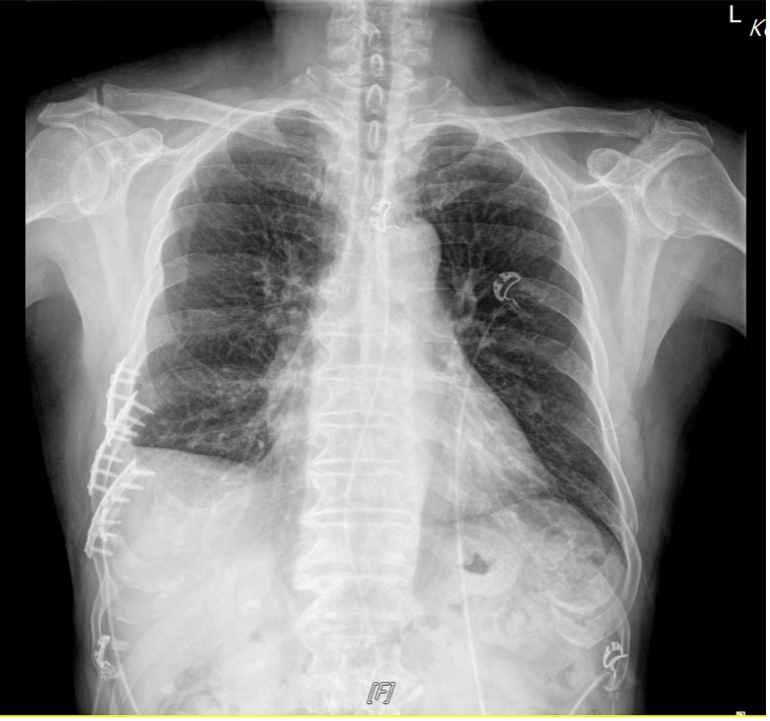
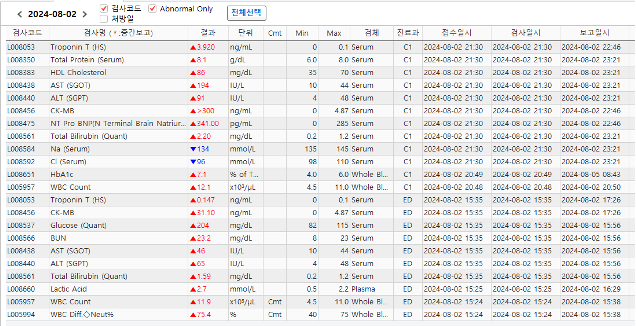
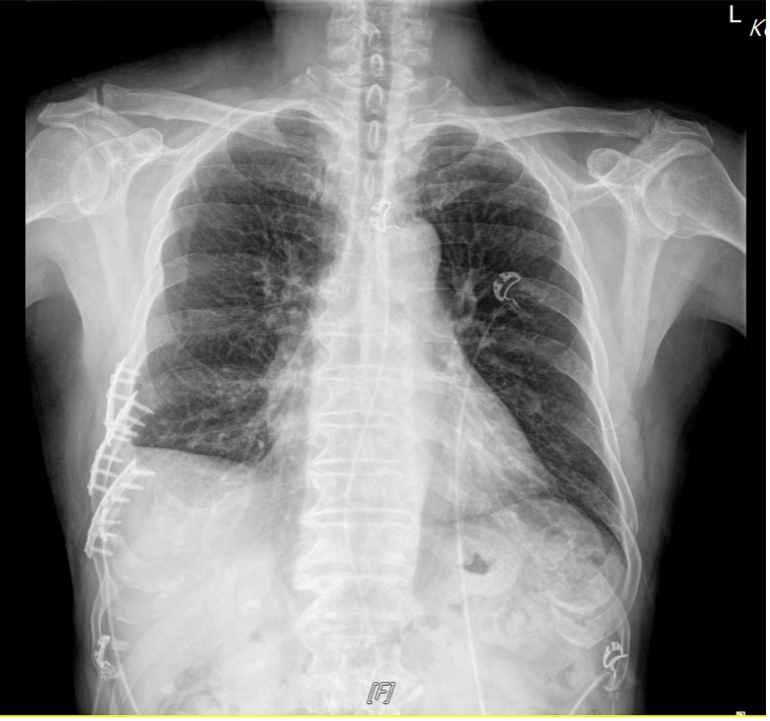
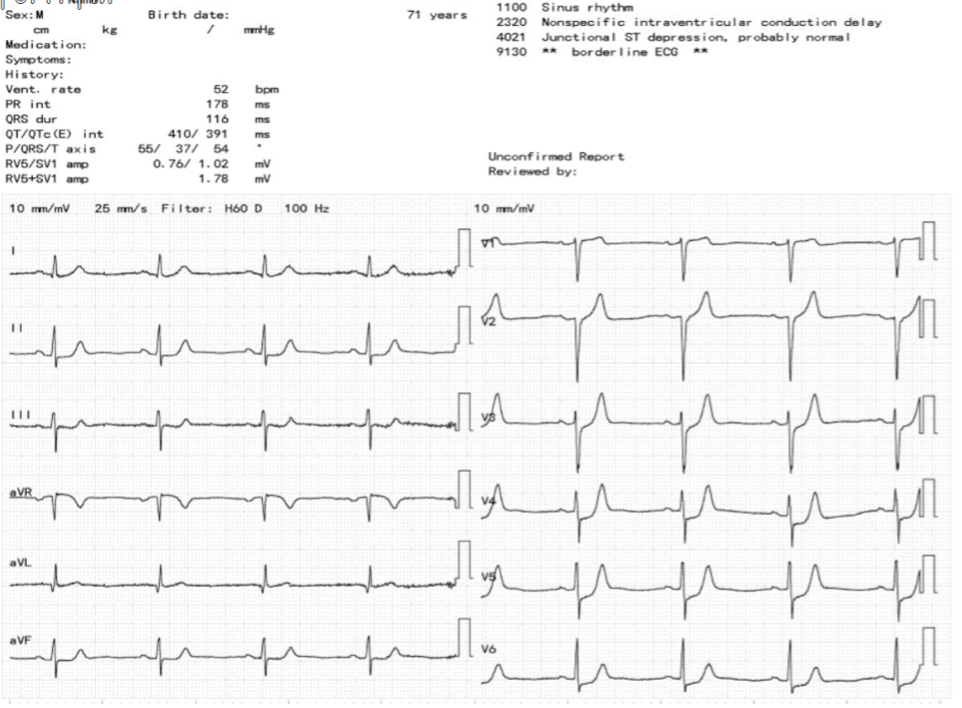
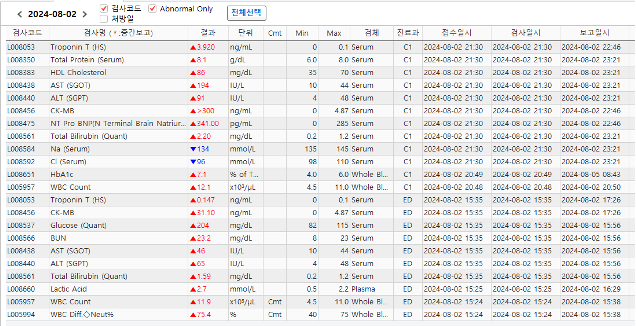
Relevant Test Results Prior to Catheterization
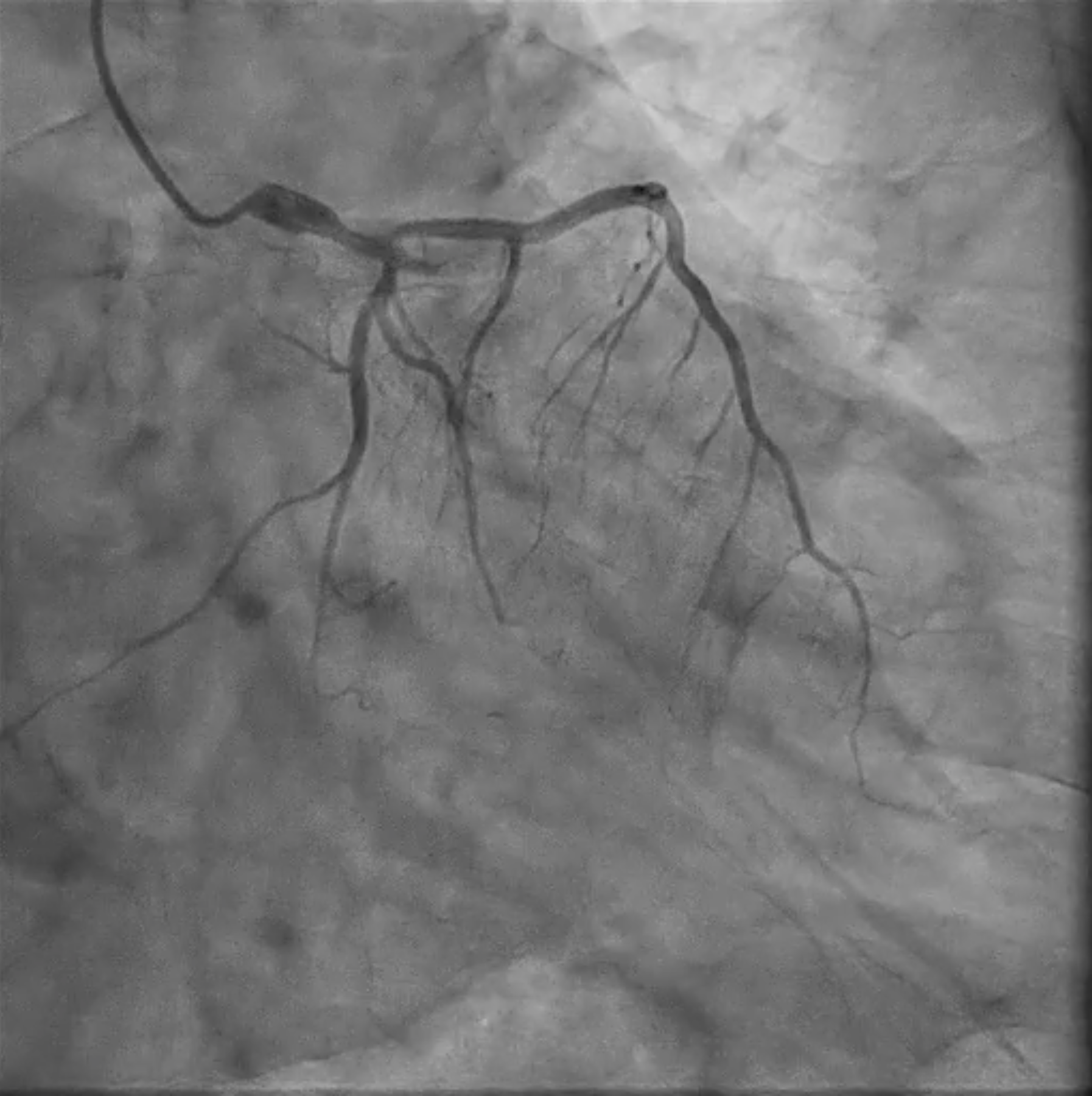
Chest x-ray showed cardiomegaly. Electrocardiogram showed ST-Depression in II, V4-6 leads and slight ST-Elevation in aVR lead. An echocardiogram revealed ischemic insult in the left anterior descending (LAD) and left circumflex (LCX). These findings showed deterioration from the previous result (EF 2019: 65%; 2024: 47%). Laboratory examination showed normal renal function and positive cardiac biomarker (hs-Trop T: 0.147 3.920 ng/mL; CKMB 31.1 >300 ng/mL).
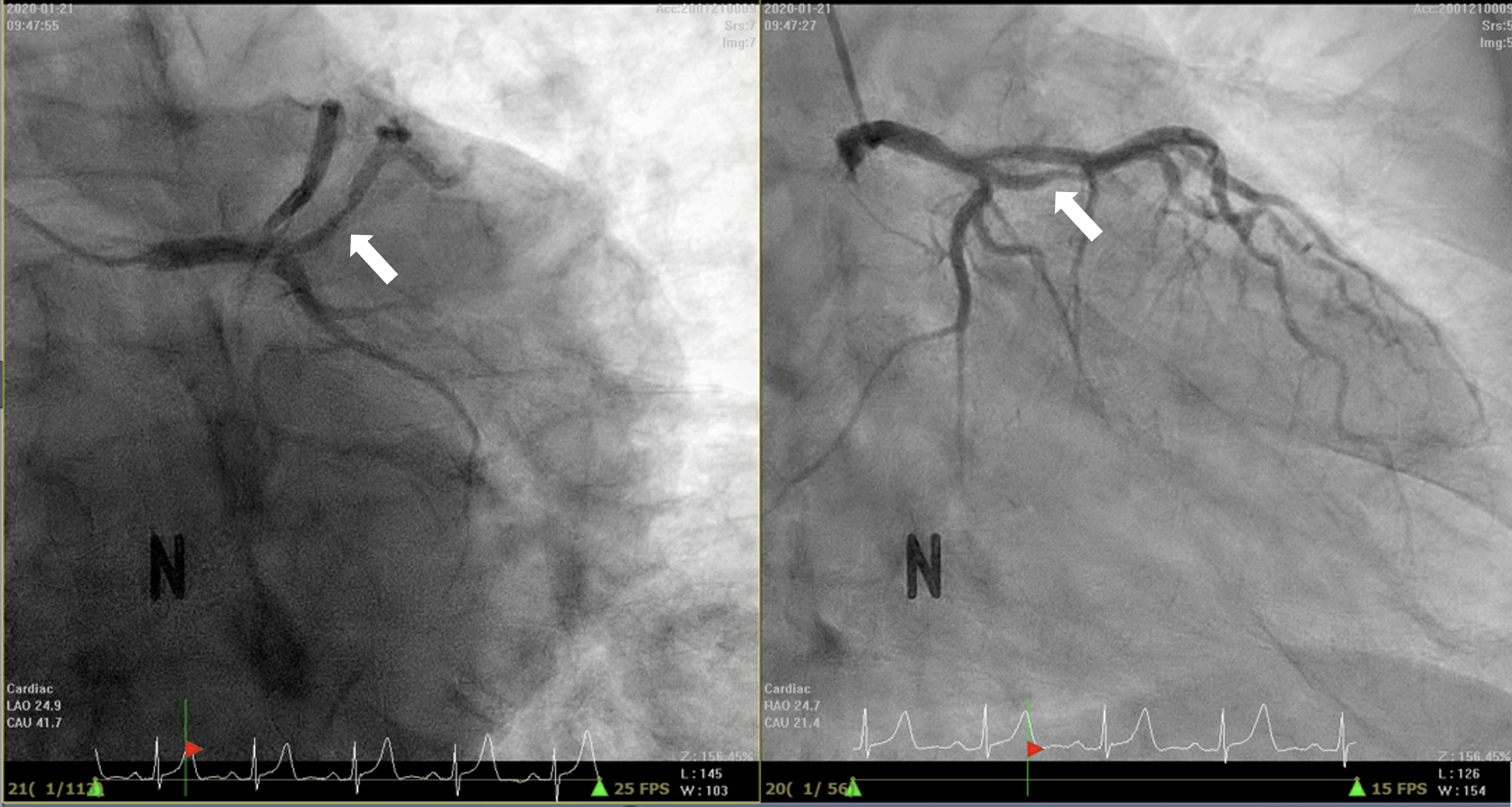
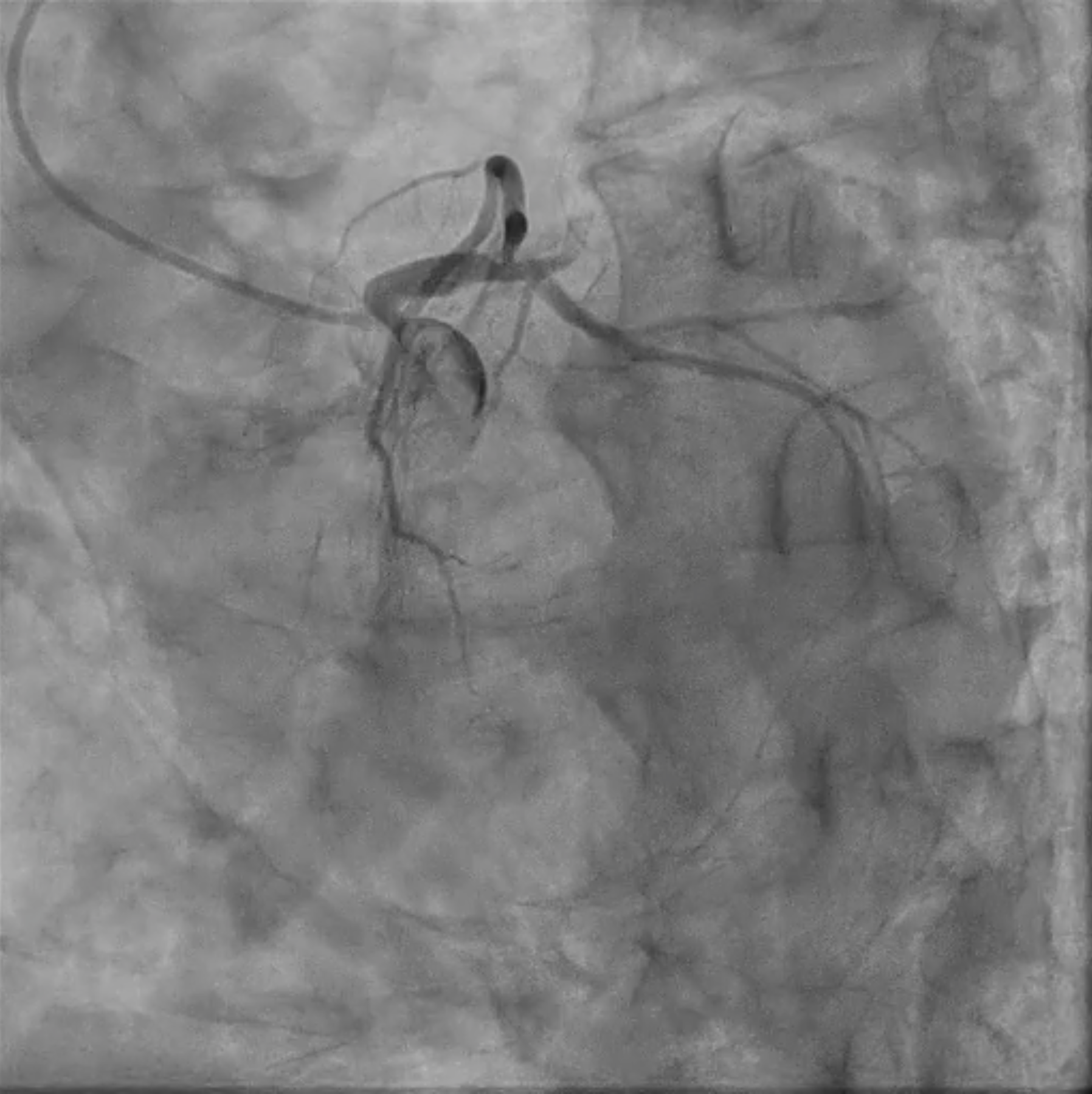
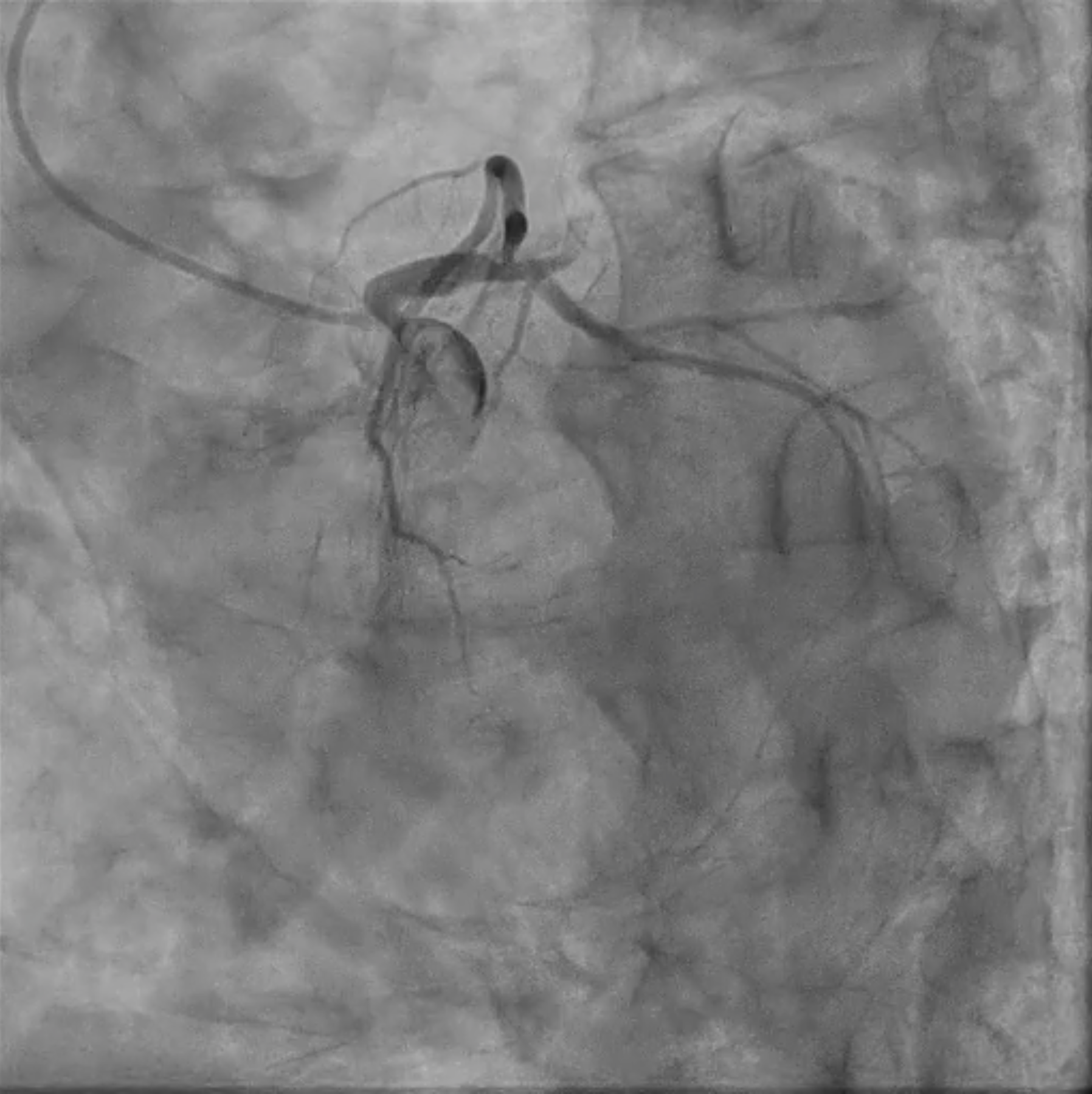
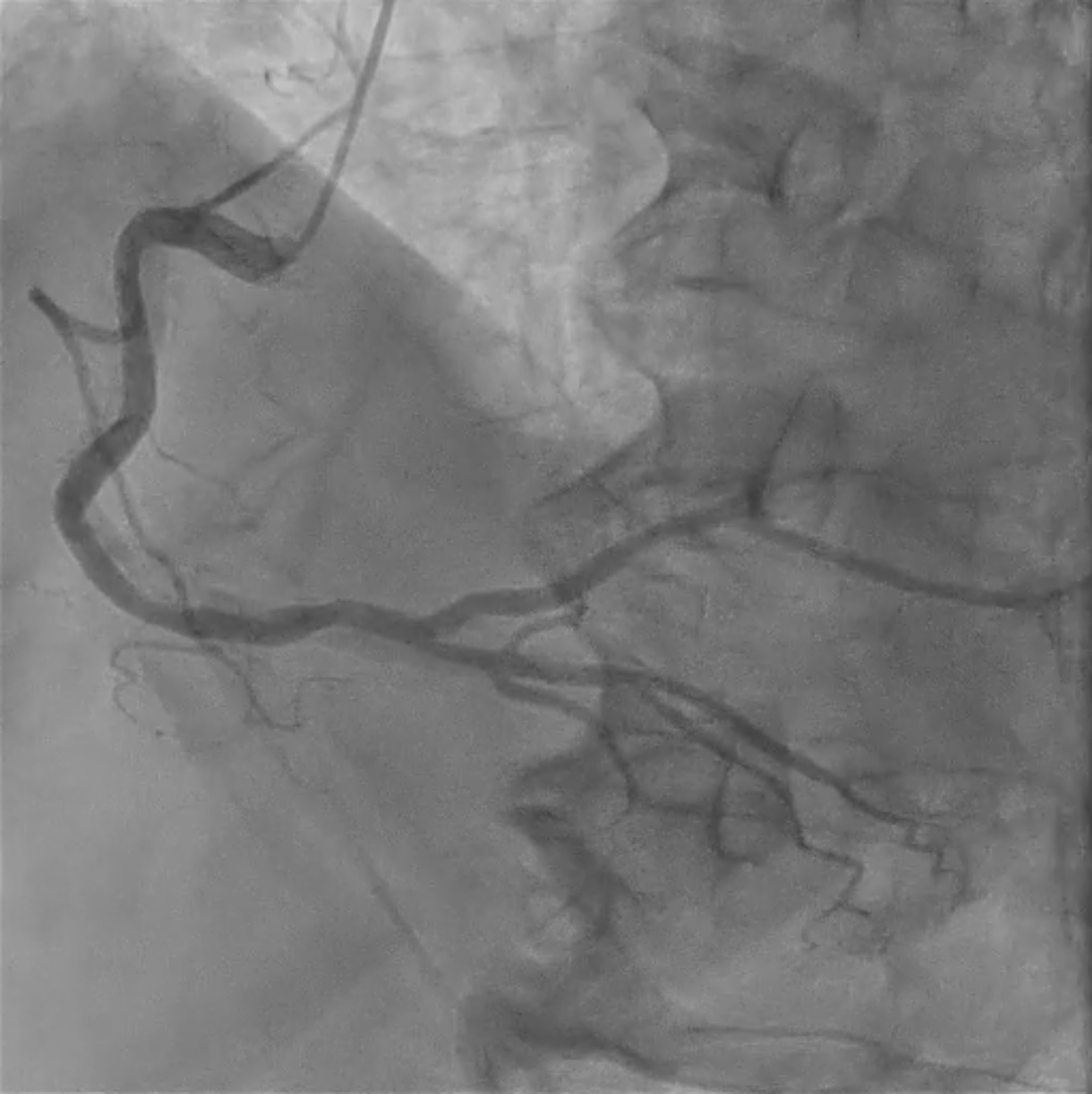
Relevant Catheterization Findings
We decided to do an early invasive strategy for this patient.
Interventional Management
Procedural Step
Runtrough guidewire under 6F EBU 3.5SH was engaged to LCA and successfully advanced to distal Ramus.
However, we observed focal dissection in the distal left main (LM), so we decided to do subsequent LM to LAD bail-out stenting.
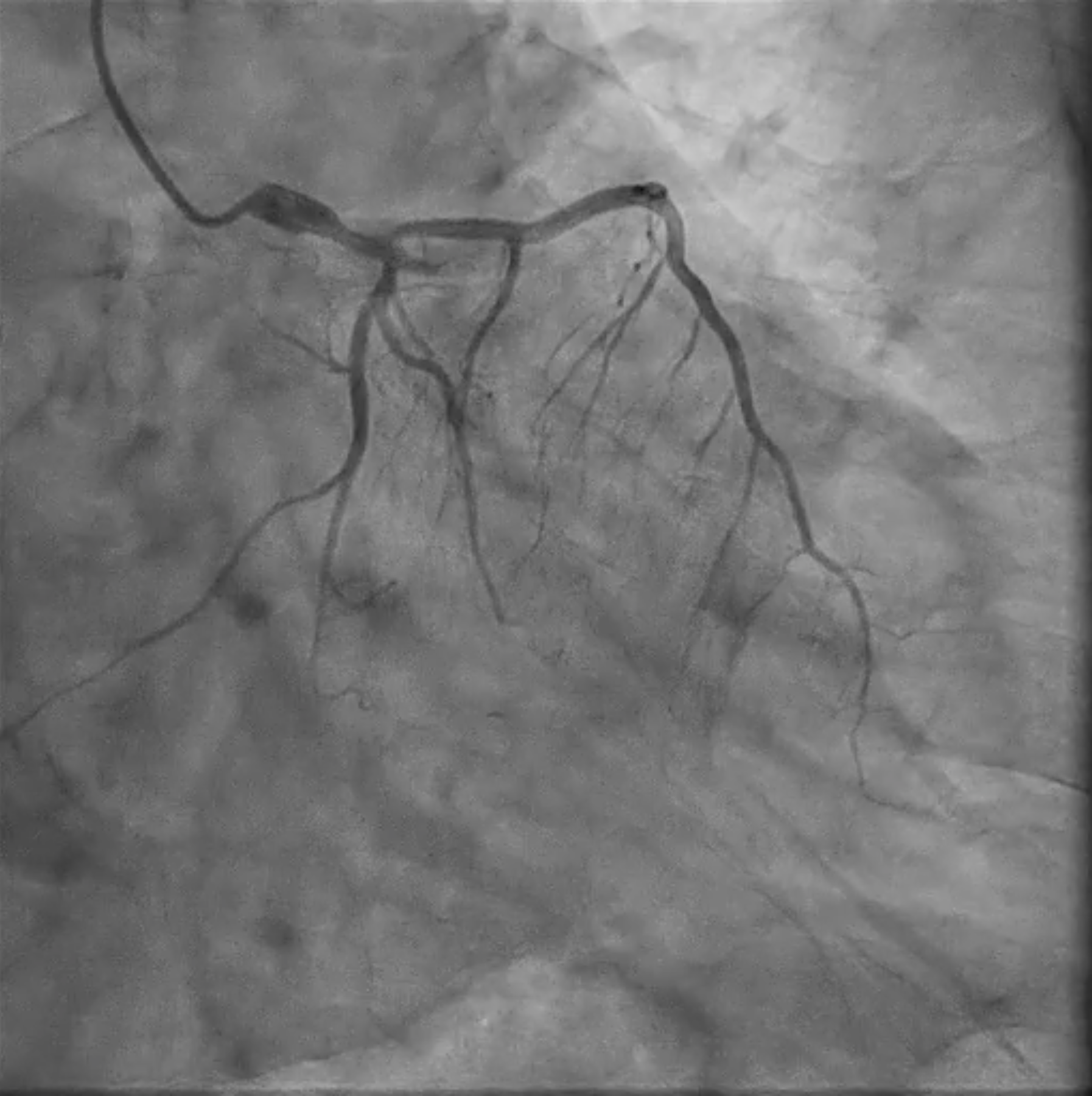
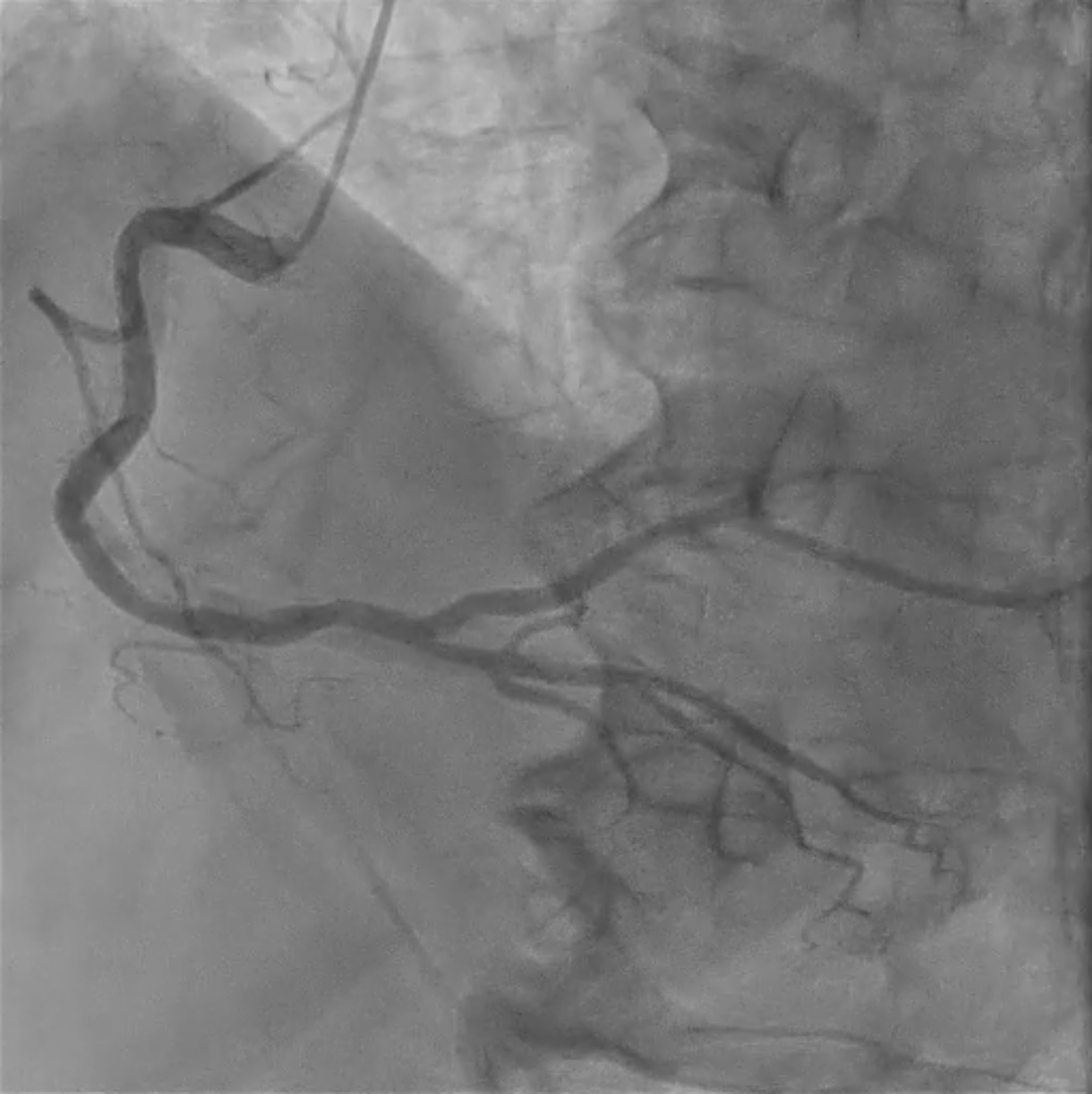
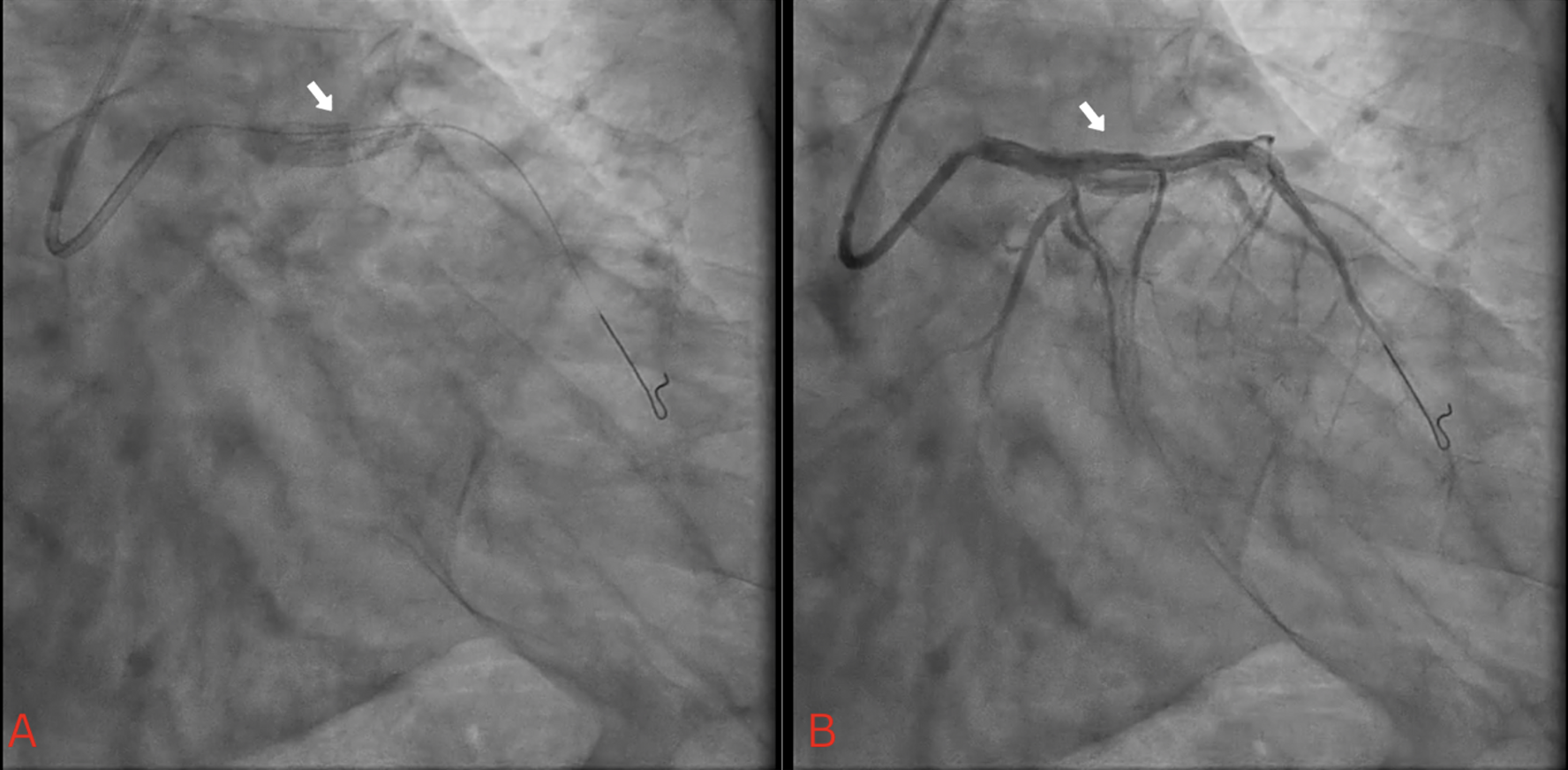
Sion guidewire under 6F EBU 3.5 SH was advanced to distal LAD. Quick pre-dilatation using ROVL 2.0/15mm (up to 8atm) showed good balloon response with residual stenosis >60%. Then, we delivered Firehawk 3.5/13mm but failed due to eccentric calcium. Buddy wire using Runtrough and Sion Blue ES also failed. Then, stent delivery was done using a 6F Telescope guide extension catheter and stent positioning was attempted by pulling back. During the stent pull back to LM, the stent balloon partly came out from the undeployed stent with high suspicious stent loss by stent entrapment. We inflated the stent directly; however, the stent balloon could not enter to distal unexpanded stent. We did gradual balloon dilation using ROVL 2.0/15mm and stent balloon 3.5/13mm from LAD stent up to distal edge LM stent.Additional stenting from ostial to distal LM was done with Firehawk 4.0/13mm. Then, we finalized with NC ROVL 3.5/9mm (up to 28atm) with a good result, TIMI3 Flow.
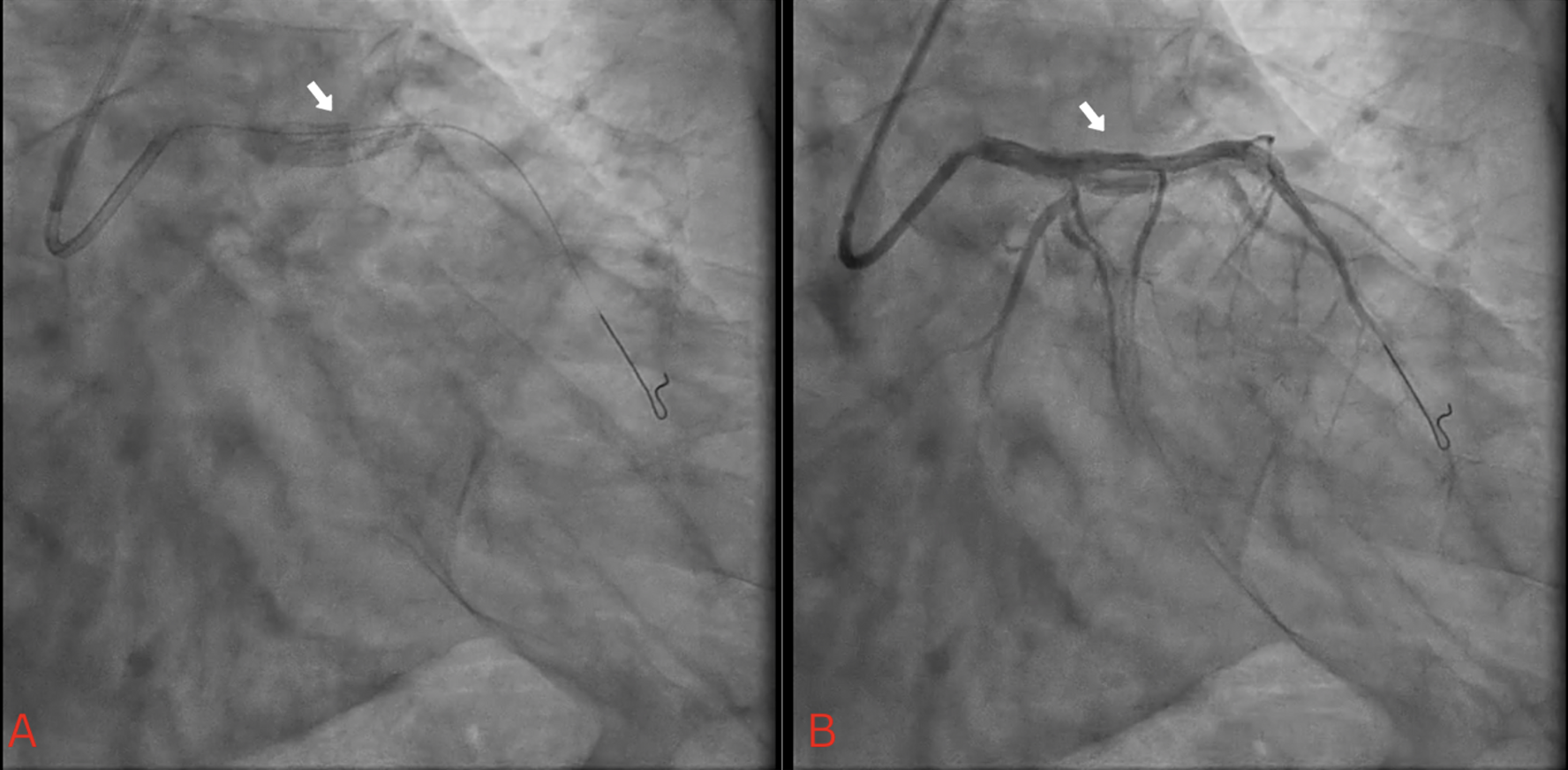
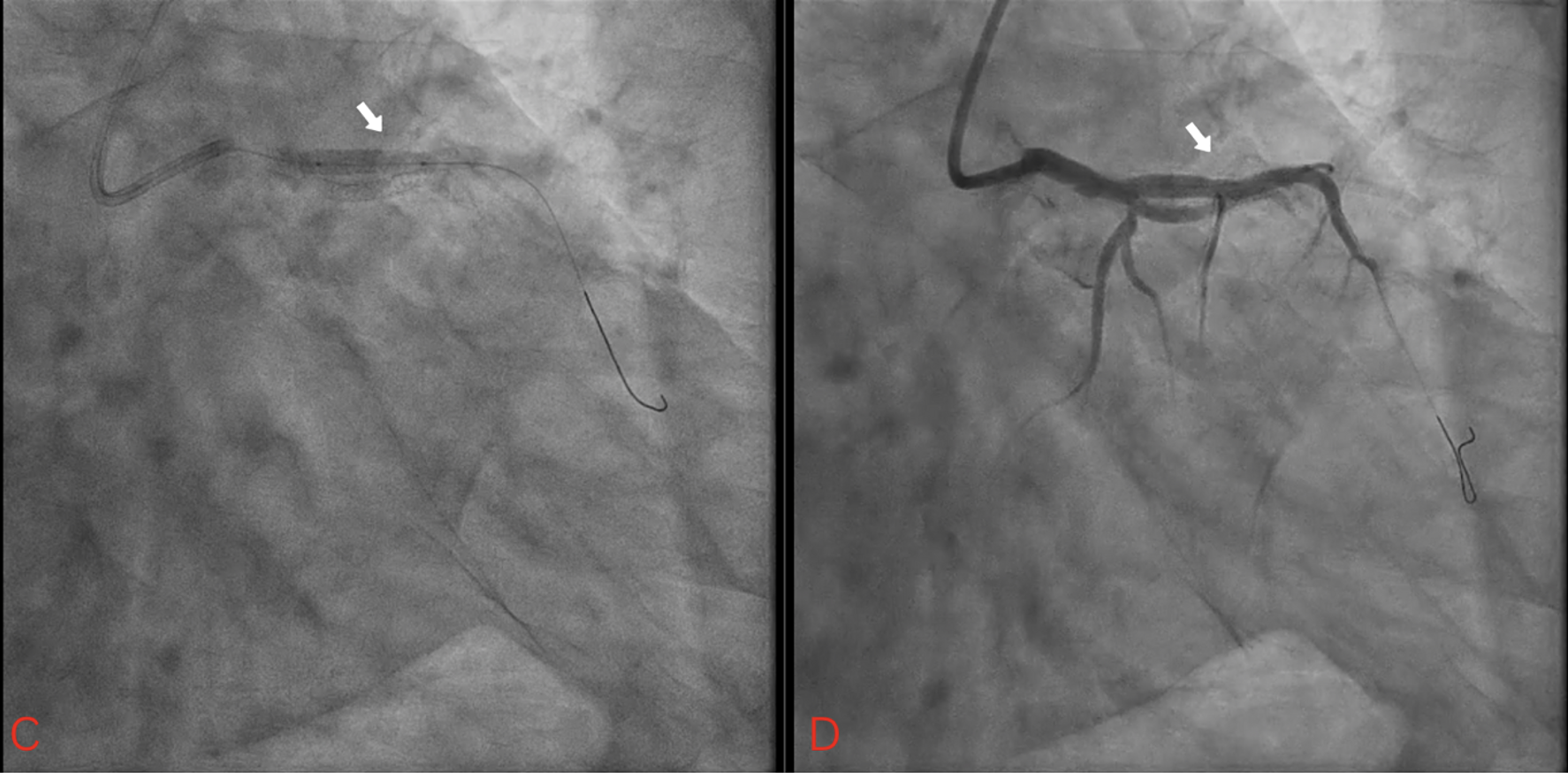
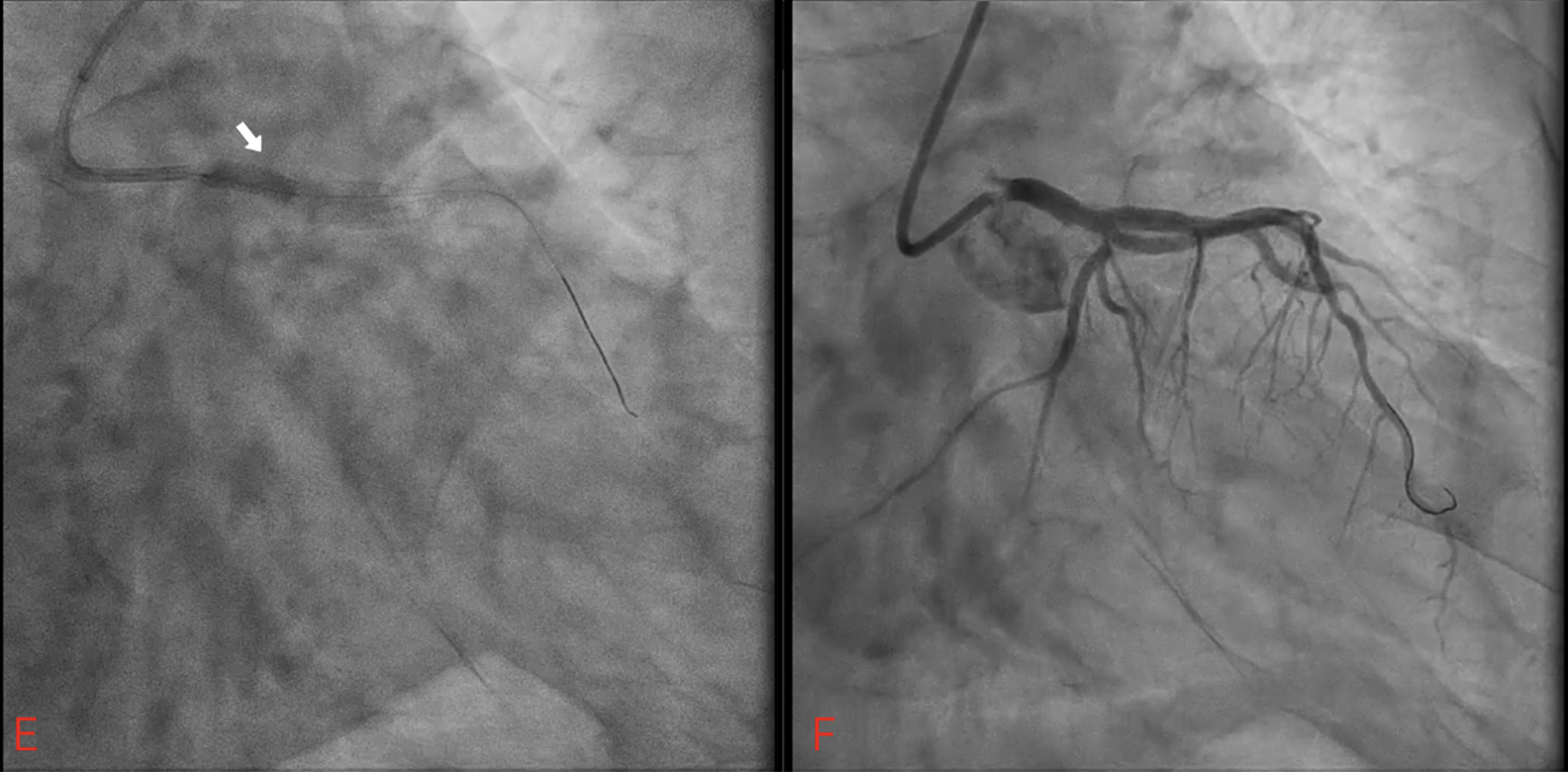
However, we observed focal dissection in the distal left main (LM), so we decided to do subsequent LM to LAD bail-out stenting.
Sion guidewire under 6F EBU 3.5 SH was advanced to distal LAD. Quick pre-dilatation using ROVL 2.0/15mm (up to 8atm) showed good balloon response with residual stenosis >60%. Then, we delivered Firehawk 3.5/13mm but failed due to eccentric calcium. Buddy wire using Runtrough and Sion Blue ES also failed. Then, stent delivery was done using a 6F Telescope guide extension catheter and stent positioning was attempted by pulling back. During the stent pull back to LM, the stent balloon partly came out from the undeployed stent with high suspicious stent loss by stent entrapment. We inflated the stent directly; however, the stent balloon could not enter to distal unexpanded stent. We did gradual balloon dilation using ROVL 2.0/15mm and stent balloon 3.5/13mm from LAD stent up to distal edge LM stent.Additional stenting from ostial to distal LM was done with Firehawk 4.0/13mm. Then, we finalized with NC ROVL 3.5/9mm (up to 28atm) with a good result, TIMI3 Flow.
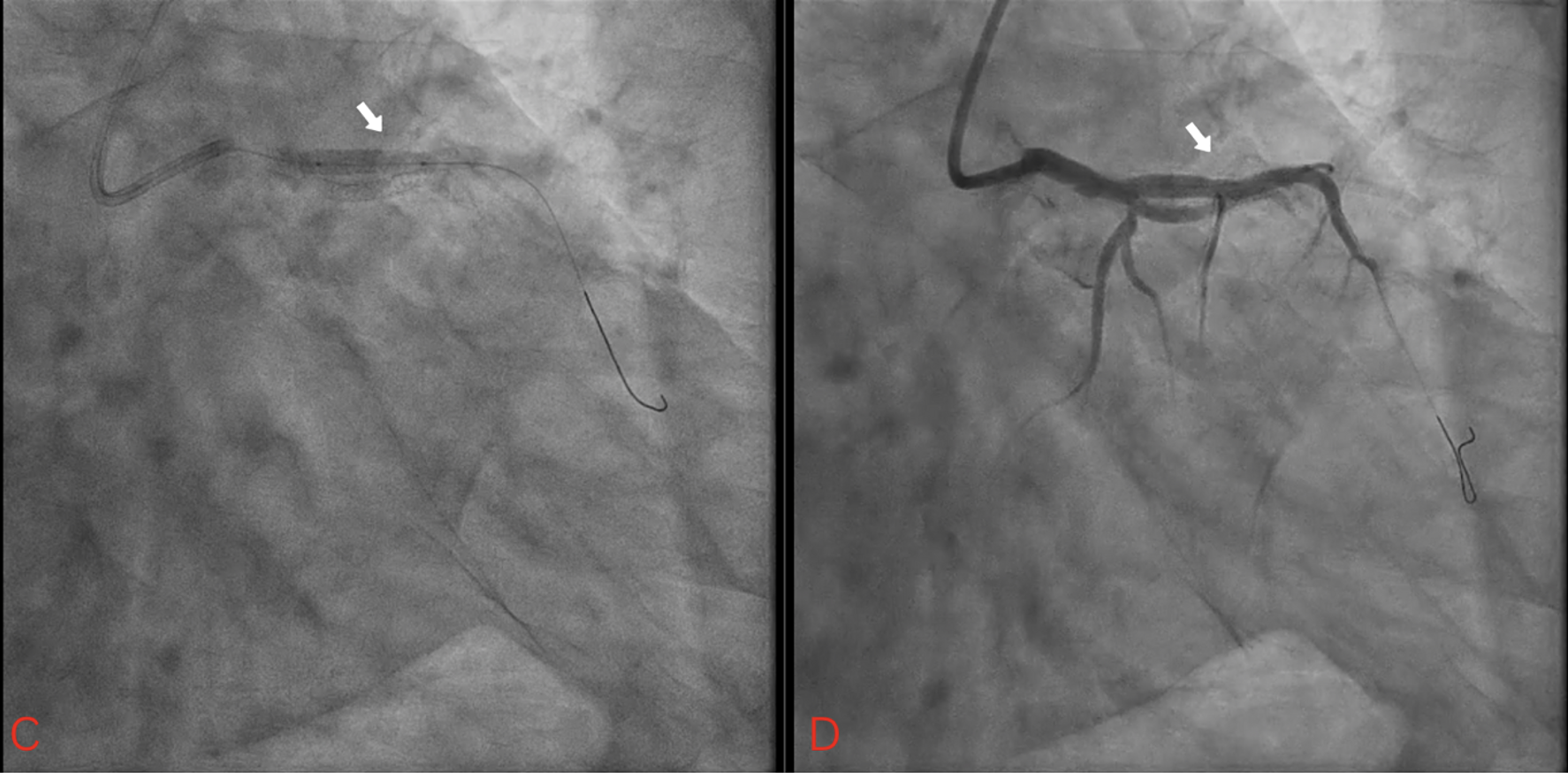
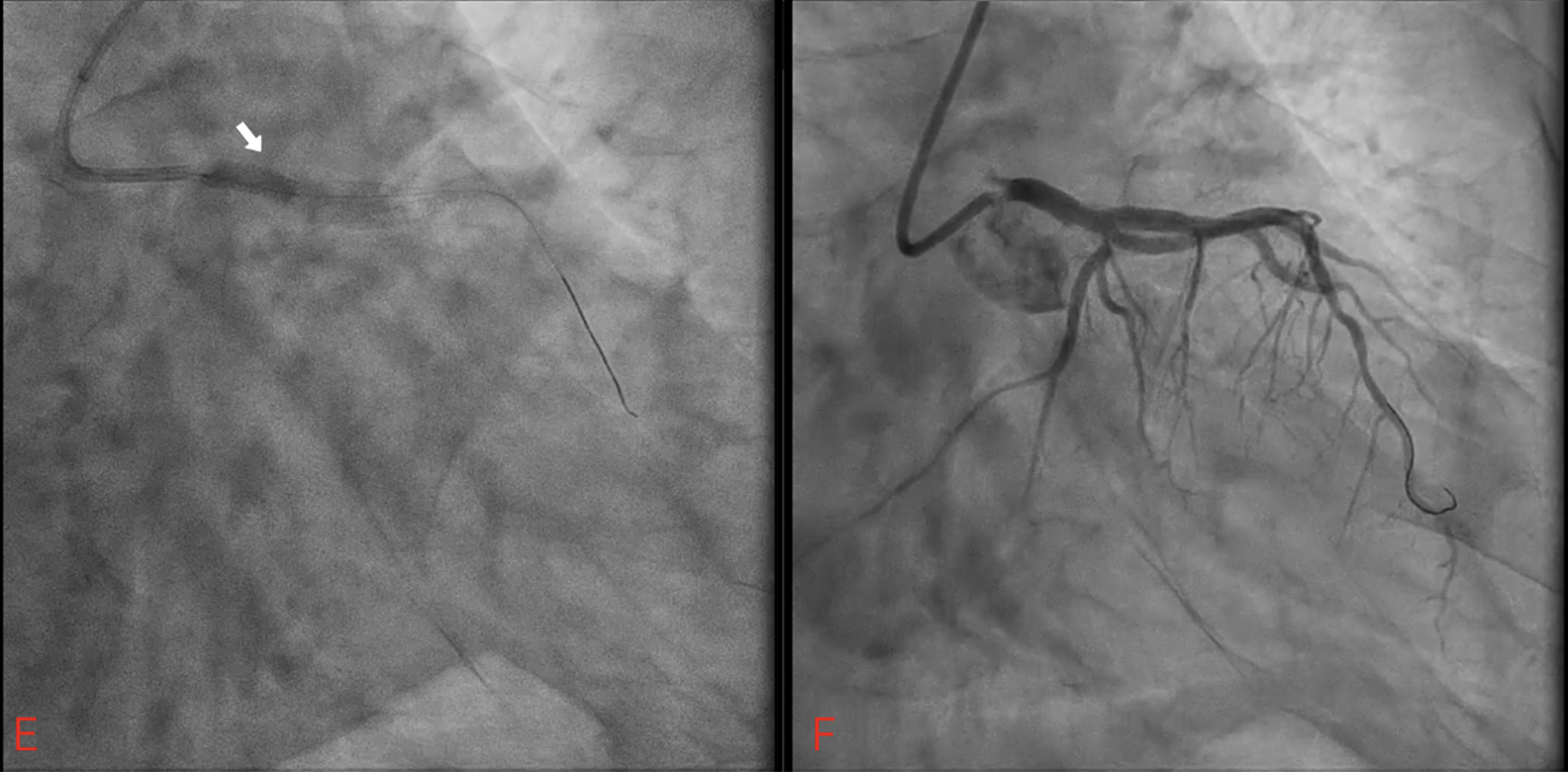
Case Summary
Failure to deliver a stent to the target site occurs in 3.9%–8.3% of the procedures, mostly due to excessive tortuosity, and calcification of the target lesion and the proximal vessel segments. This maylead to stent dislodgement from the delivery balloon catheter and subsequent stent embolization/loss. We did a modified small-diameter balloon catheter technique to expand the distal part of the mid-LAD stent followed by bail-out stenting to LM-LAD. This technique requires experienced operators and quick decision-making in AMI management to prevent further complications such as embolization or acute in-stent thrombosis.
