CASE20240809_004
Double Uncommon Situation in Acute ST-Elevation Myocardial Infarction
By Thitima Limjaroen
Presenter
Thitima Limjaroen
Authors
Thitima Limjaroen1
Affiliation
King Chulalongkorn Memorial Hospital, Thailand1,
View Study Report
CASE20240809_004
ACS/AMI - ACS/AMI
Double Uncommon Situation in Acute ST-Elevation Myocardial Infarction
Thitima Limjaroen1
King Chulalongkorn Memorial Hospital, Thailand1,
Clinical Information
Relevant Clinical History and Physical Exam
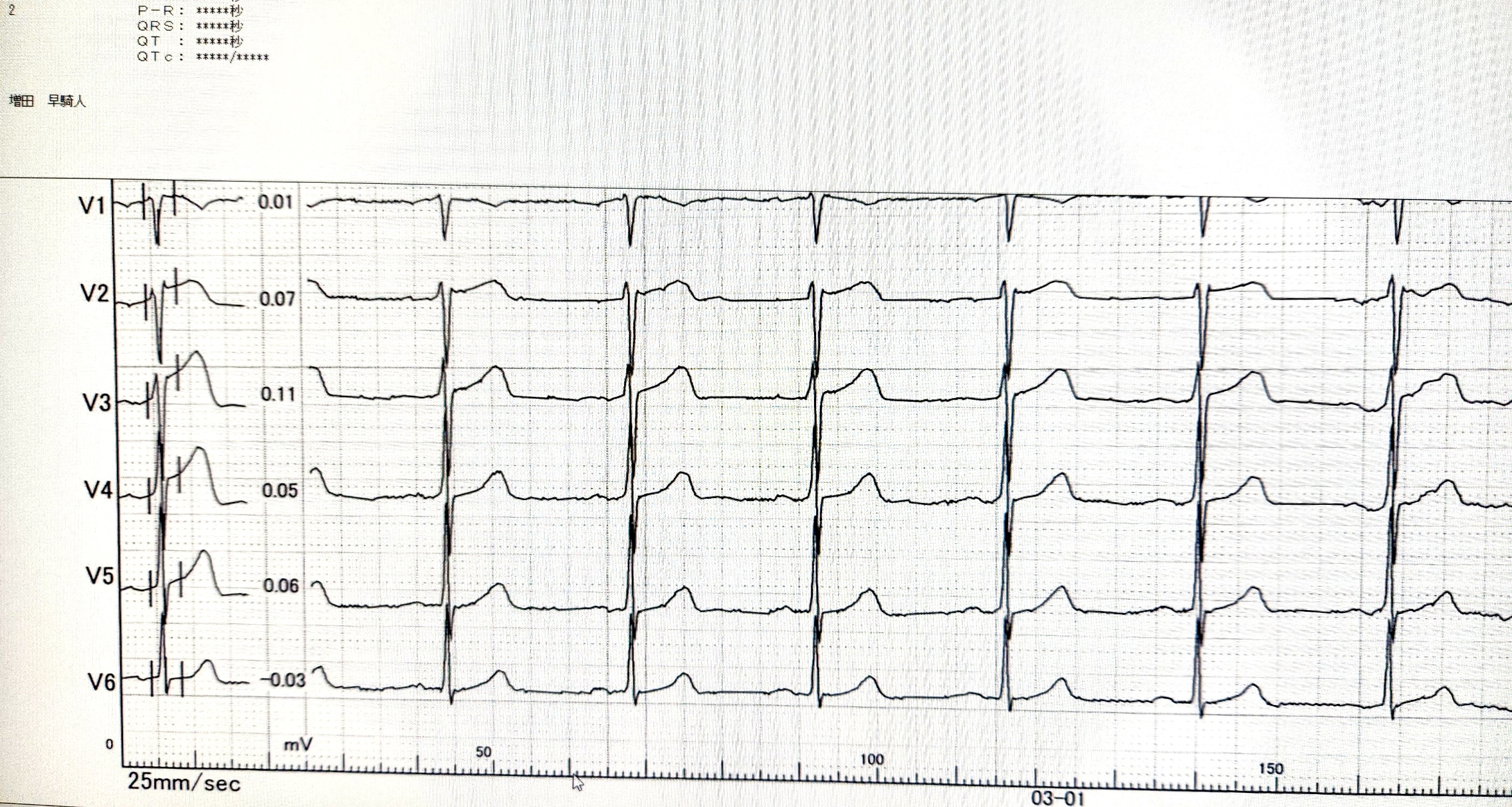
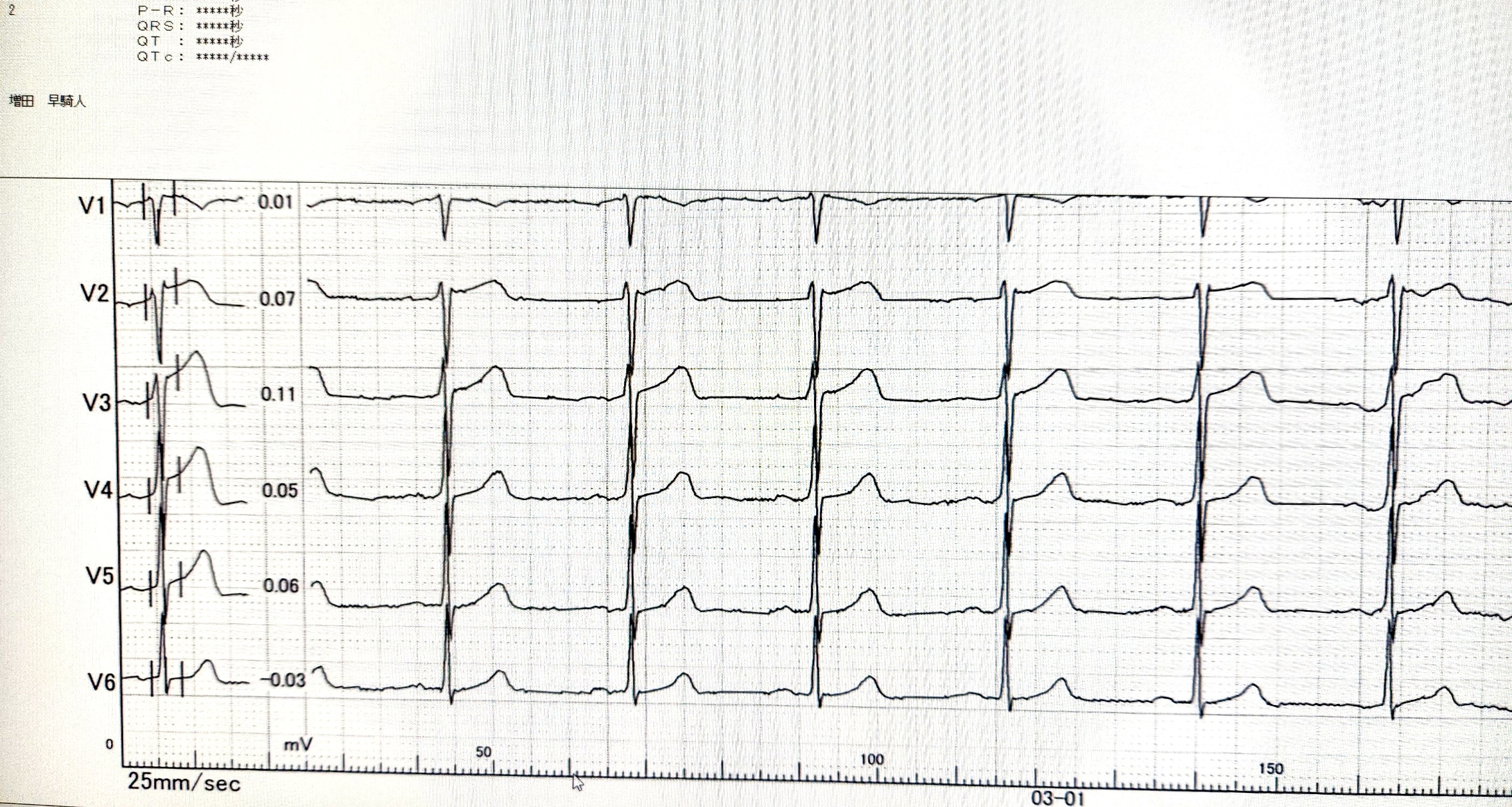
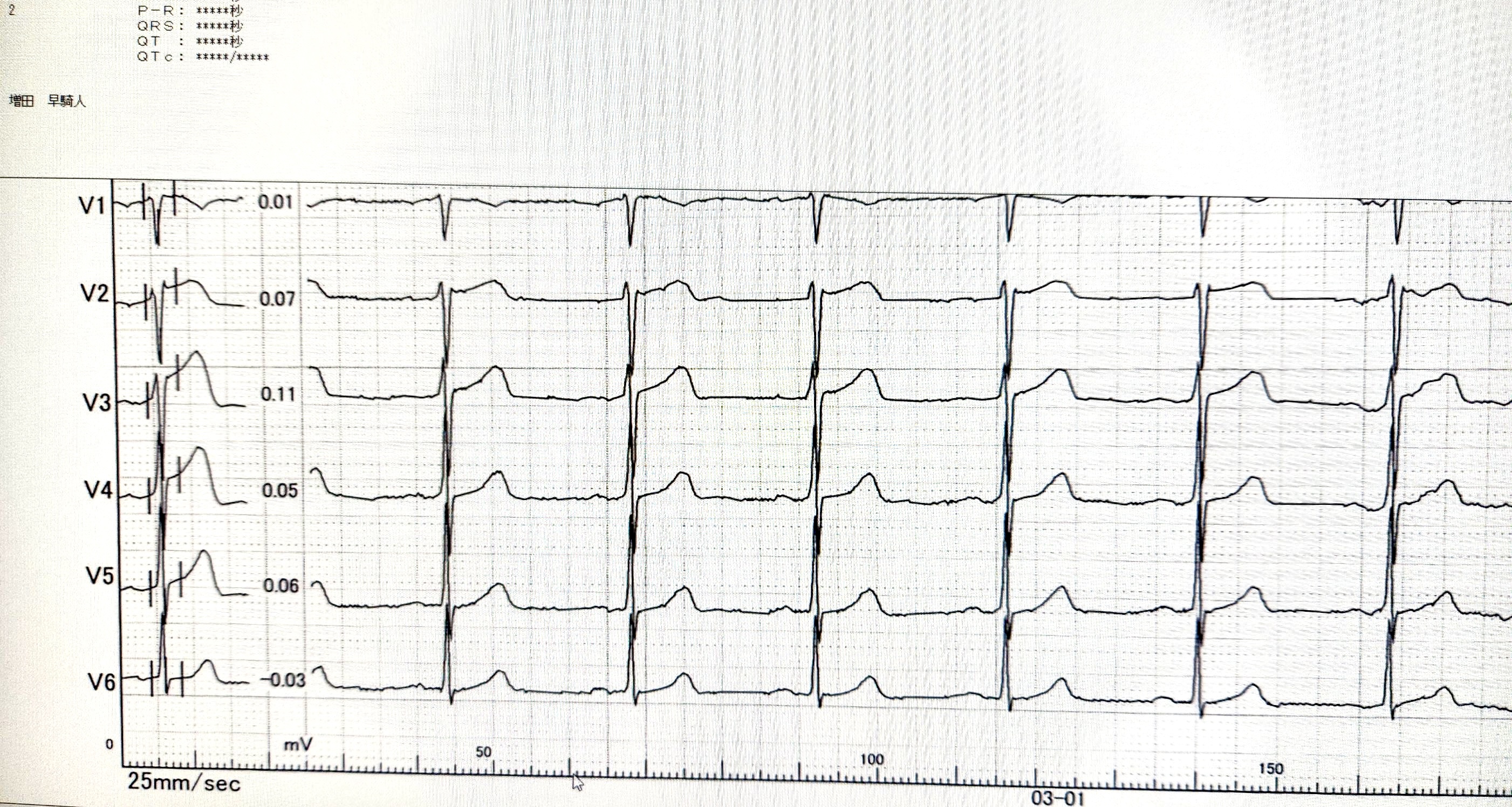
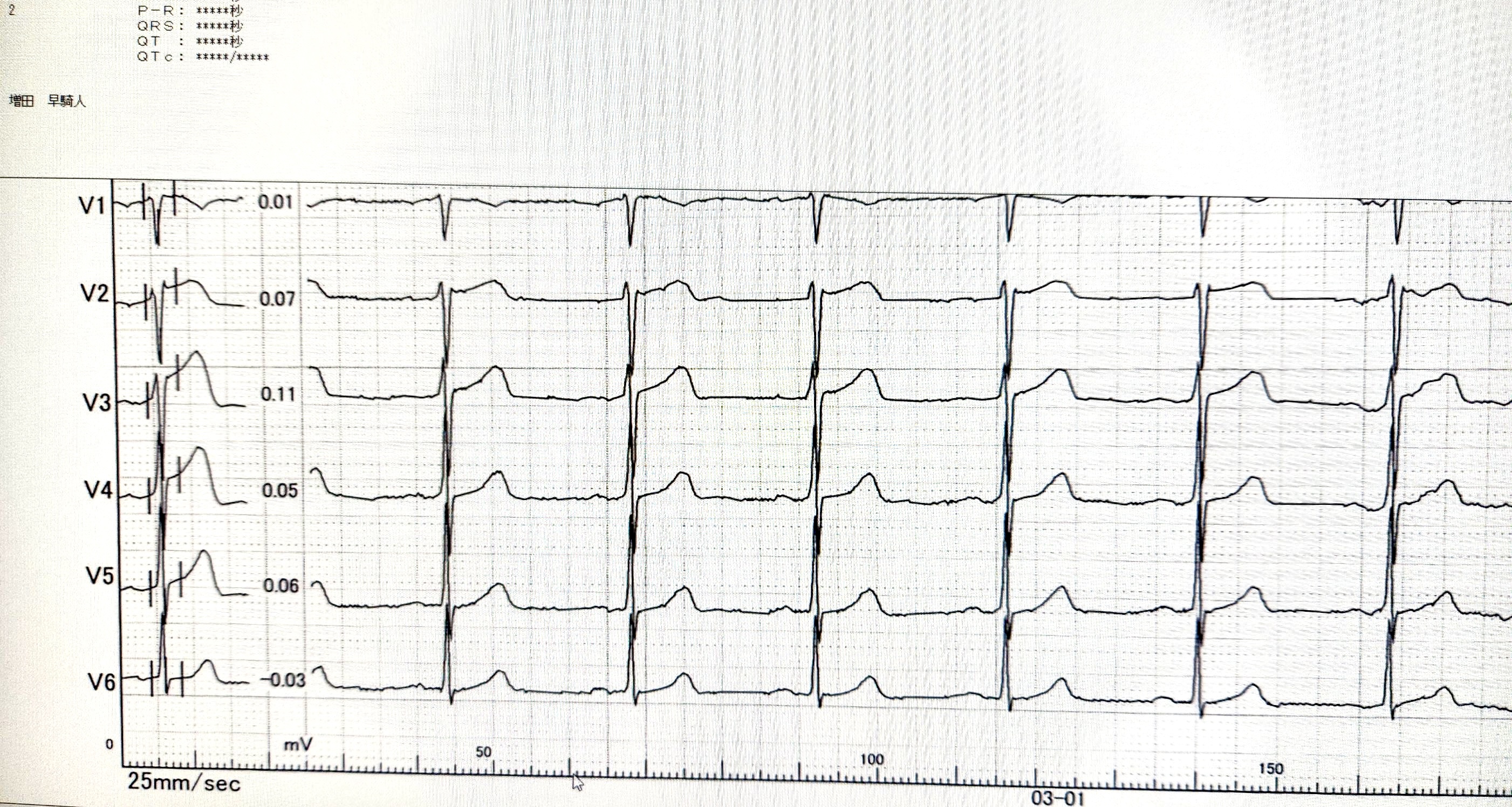
A 47-year-old woman presented to the emergency department complaining of spontaneous and severe retrosternal pain radiating to the left arm. The patient had no history of hypertension, diabetes, dyslipidemia, smoking, or familial heart disease. Physical examination was unremarkable. Blood pressure and heart rate were within the normal range, and blood pressure was not significantly different between the right and left hands. The presentation's initial electrocardiogram (ECG) revealed anterior ST-segment changes (V2-V4 leads).
Relevant Test Results Prior to Catheterization
Laboratory tests were normal except for an elevated serum troponin level. Echocardiography displayed a normal left ventricular ejection fraction and hypokinesia of the apex and septal wall of the left ventricle.
Relevant Catheterization Findings
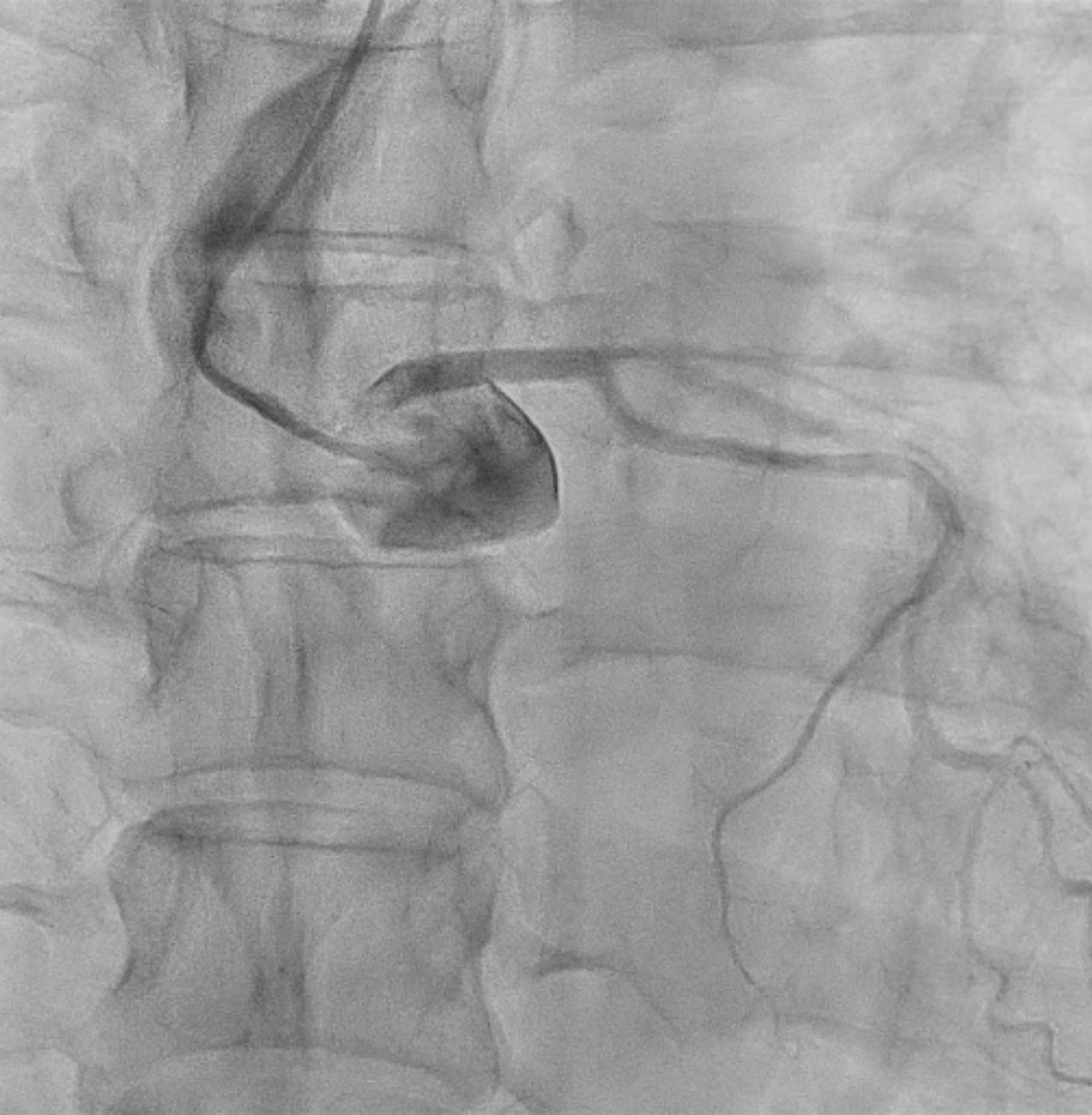
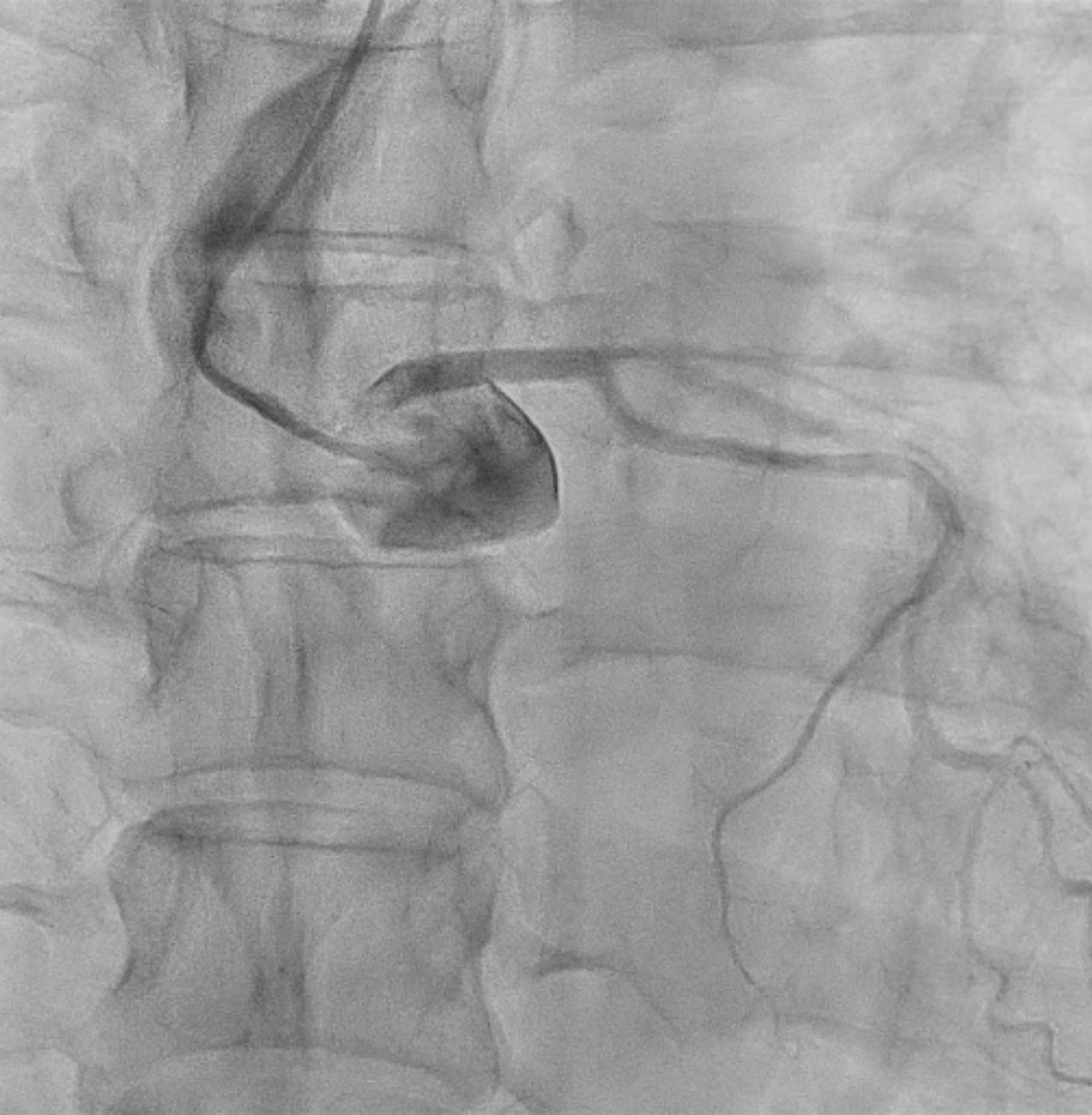
The angiography revealed a normal right coronary artery. However, attempts to cannulate the left coronary artery were not successful using diagnostic catheters, as well as the JL 3.5, JL 3.0, JL 1, and AL 1. A JR 4 diagnostic catheter was decided to be positioned as near as possible to the left coronary artery, and a Sion blue guide wire was subsequently used to cannulate the left coronary artery. The angiogram showed total occlusion from mid to distal LAD.
 Coronary_15_fps_Low_6_11.mp4
Coronary_15_fps_Low_6_11.mp4
Interventional Management
Procedural Step
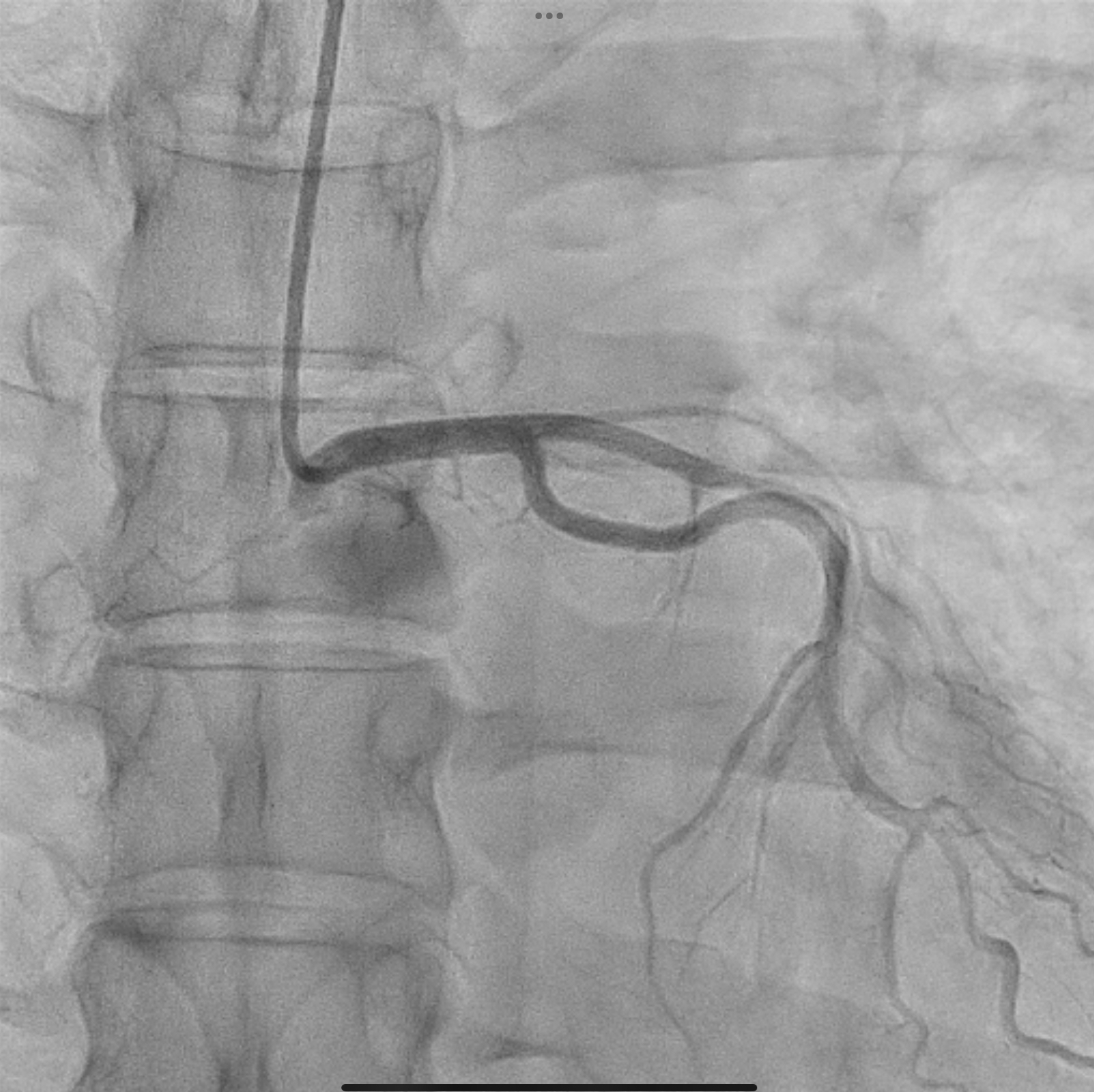
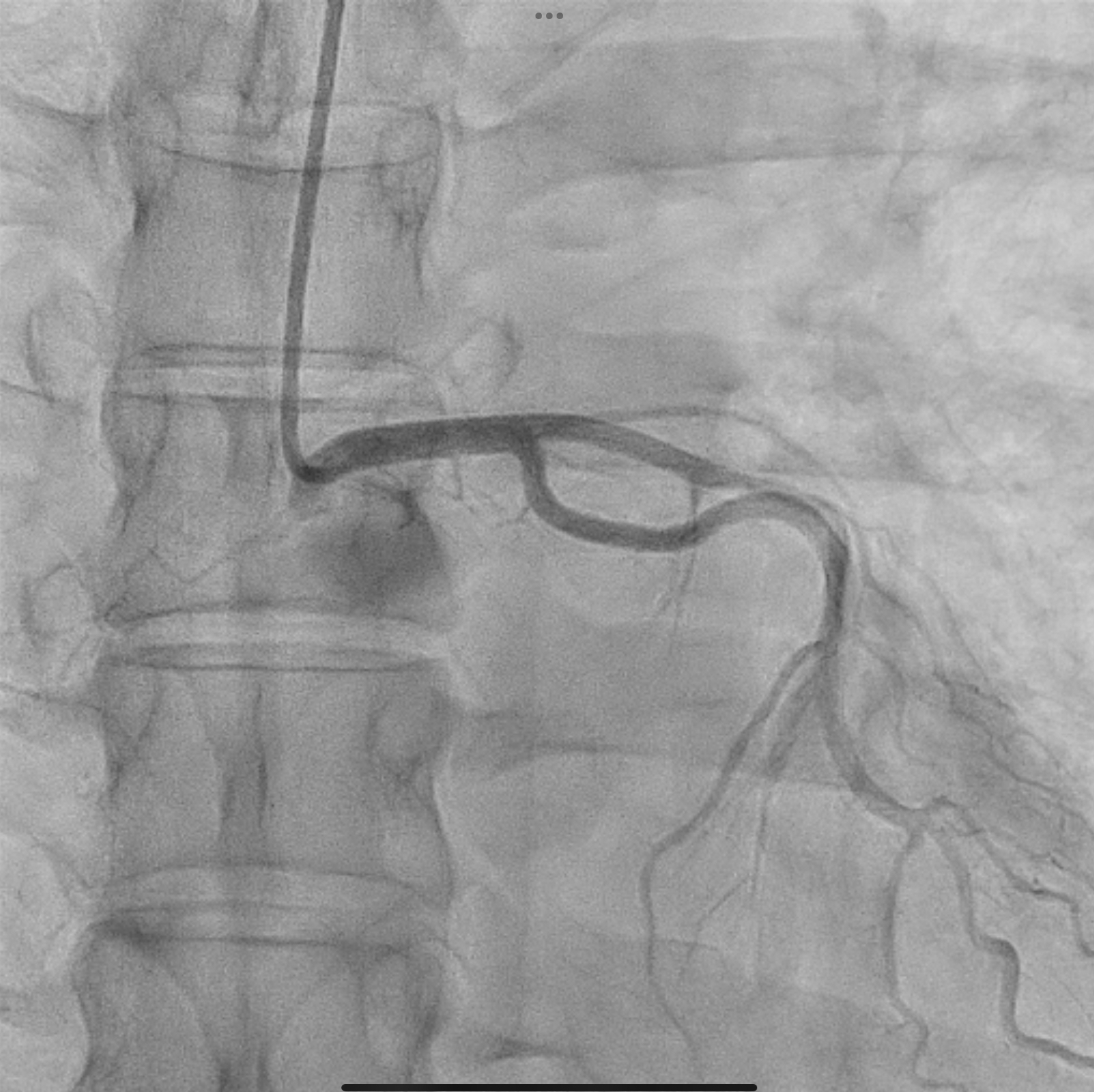
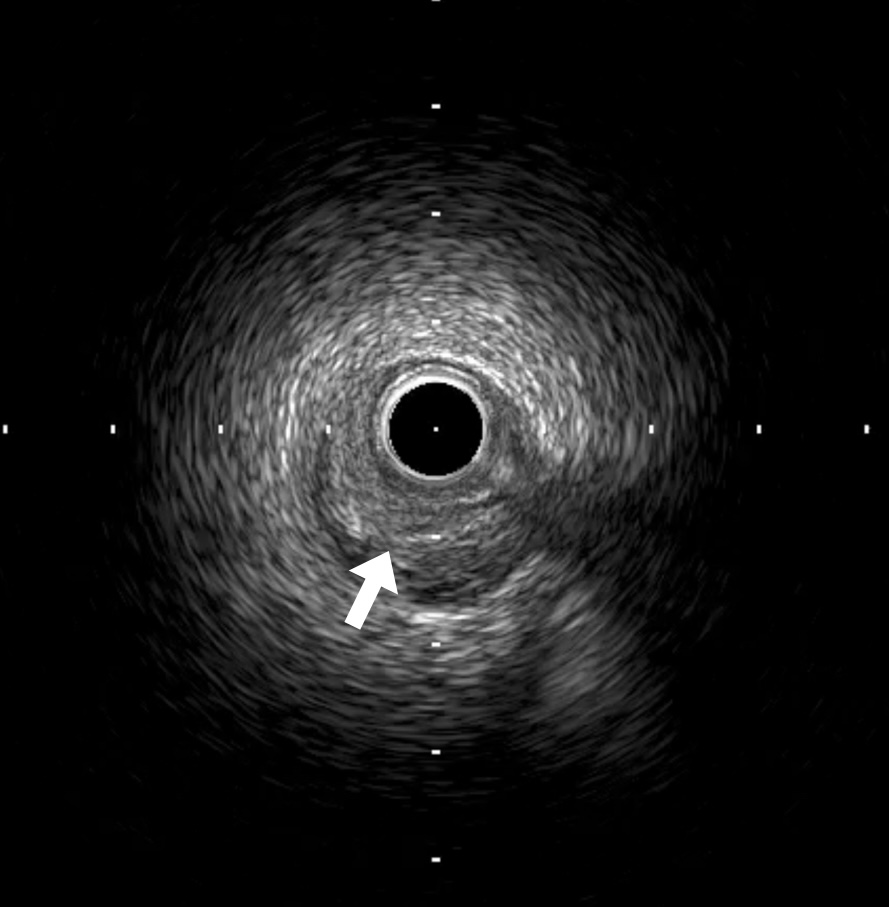
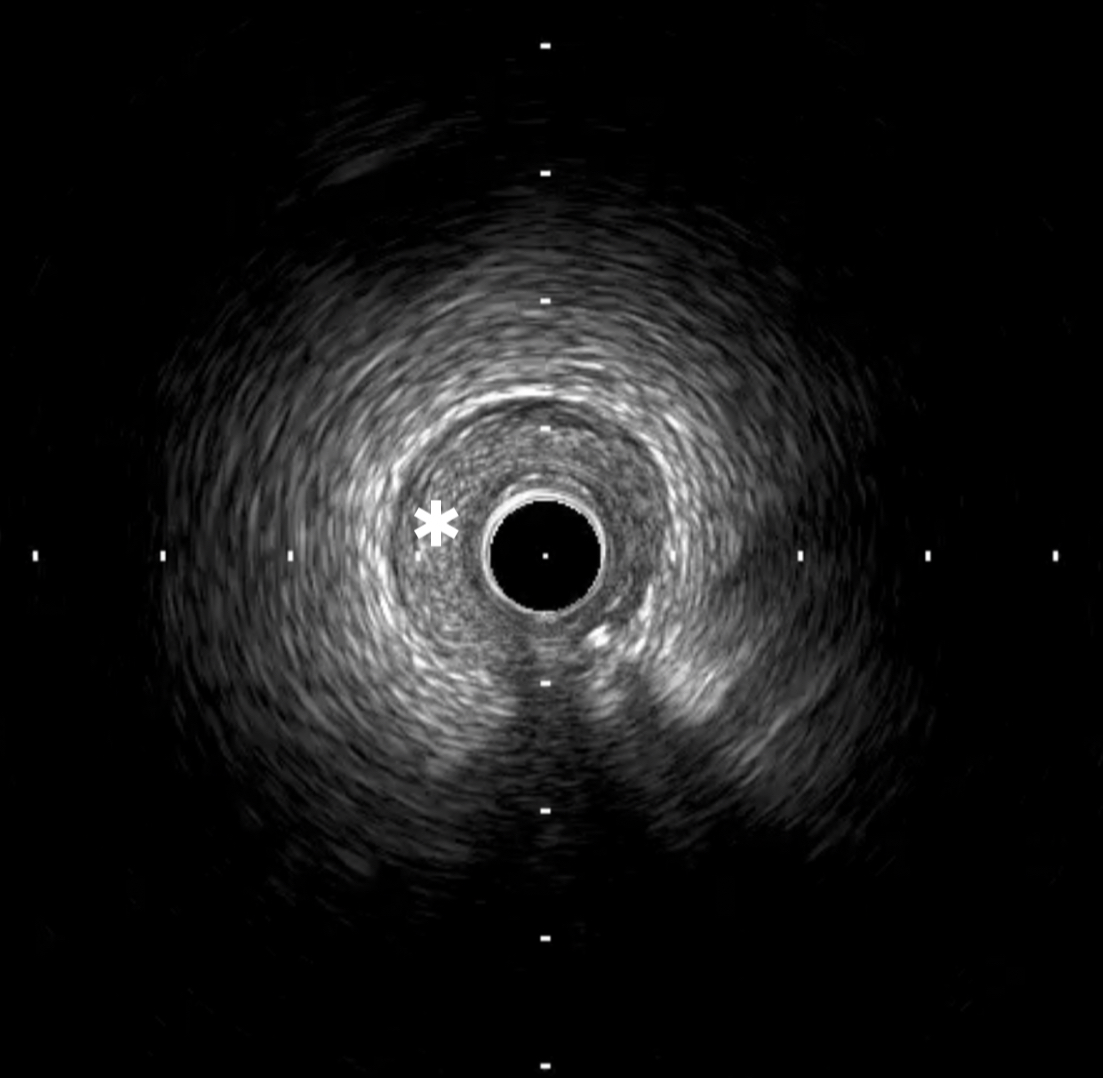
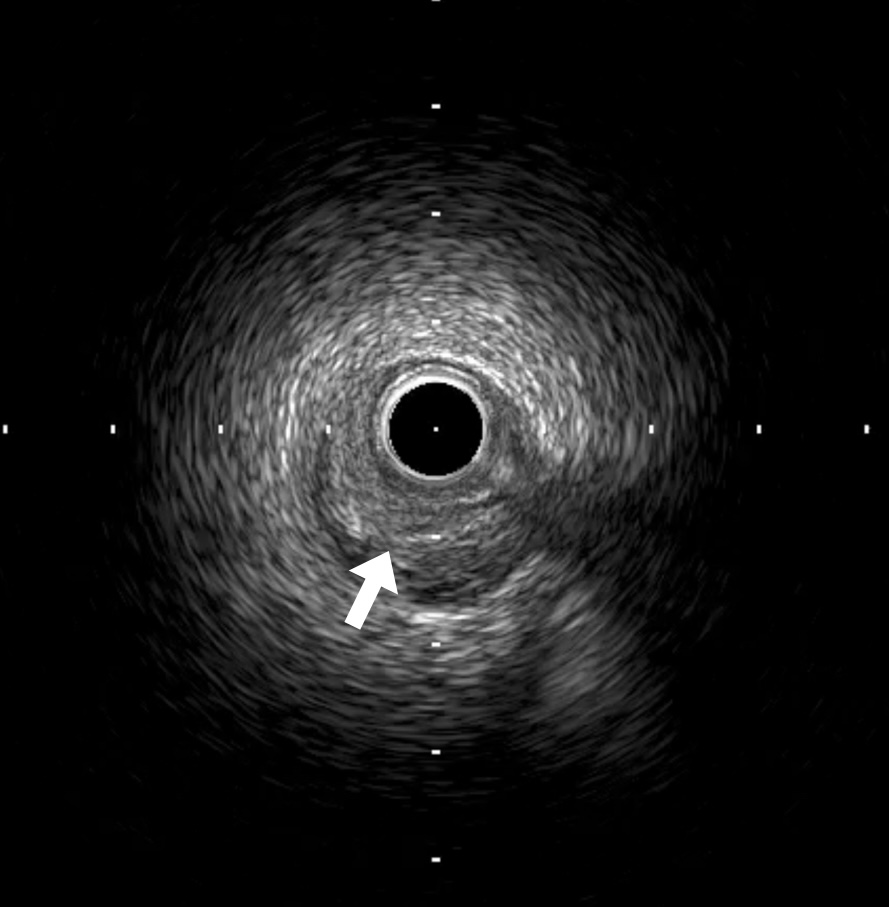
A 300 cm Gran Slam wire and 130 cm microcatheter were used to exchange to the internal mamillary guiding catheter. Afterward, the guide catheter was advanced to the left coronary artery using the guide wire as a rail to track the catheter to the correct position. IVUS examination showed an entry intimal tear proximal to the lesion site (arrow) and circumferential hematoma extending deep into the media (*), causing compressing of the true lumen. The compressive hematoma was treated with a 2.5 × 10 mm Wolverine Cutting Balloon at nominal pressure in the proximal part of the lesion and 2.0x10 mm at 14 atm in the distal part of the lesion to make entry to the true lumen. Following the inflations, flow to TIMI-3 to the distal artery normalized. After observing for 10 minutes, the flow was still good; thus, coronary stent placement was not required.
 Coronary_15_fps_Low_54_69.mp4
Coronary_15_fps_Low_54_69.mp4
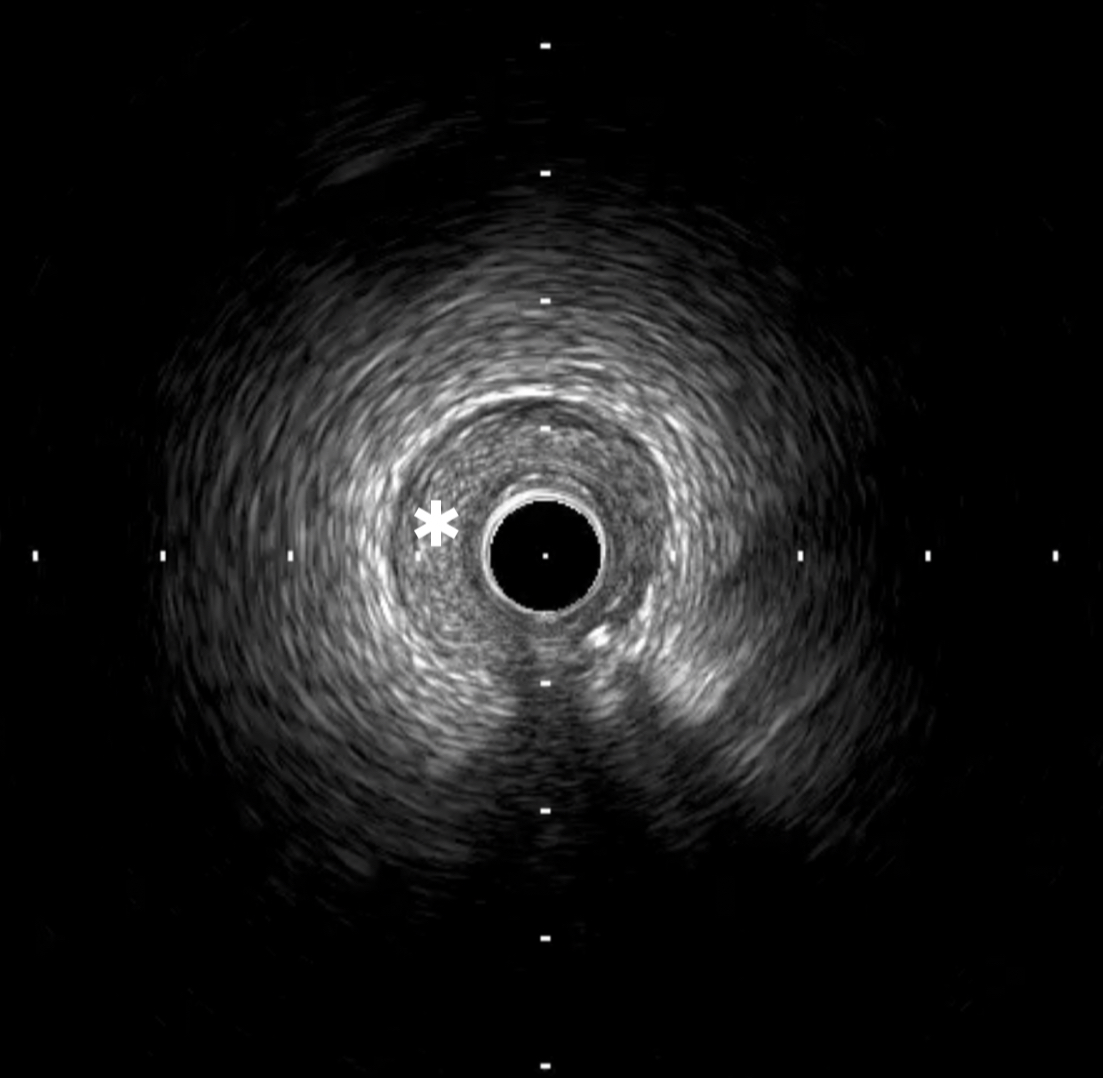
Case Summary
Coronary intervention can be considered as the first-line approach for SCAD complicated by occlusion or significantly slowed flow, especially in cases of proximal dissection or TIMI of grade 0 or 1 flow. Fenestration of the intima with the CB creates communication between the false and true lumen, enabling decompression of the intramural hematoma, thus avoiding the need for stenting. Intracoronary imaging is of great value for the diagnosis of SCAD. It is also of great importance for the guidance of angioplasty by allowing correct positioning of the wire in the right lumen, efficient inflation of the CB with multiple entry sites, and absence of insufficient expansion of the stent.
