CASE20240808_002
A Challenging Case Report : A Case of Mysterious Infarct Related Artery in a Young Patient with Extensive ST Elevation Anterolateral Wall Myocardial Infarction and Cardiogenic Shock
By Gyatso Wangchuk Bhutia, Harsha Onteddu
Presenter
Gyatso Wangchuk Bhutia
Authors
Gyatso Wangchuk Bhutia1, Harsha Onteddu1
Affiliation
Shri Siddhartha Medical College & Hospital, Tumkur, India1,
View Study Report
CASE20240808_002
ACS/AMI - ACS/AMI
A Challenging Case Report : A Case of Mysterious Infarct Related Artery in a Young Patient with Extensive ST Elevation Anterolateral Wall Myocardial Infarction and Cardiogenic Shock
Gyatso Wangchuk Bhutia1, Harsha Onteddu1
Shri Siddhartha Medical College & Hospital, Tumkur, India1,
Clinical Information
Relevant Clinical History and Physical Exam
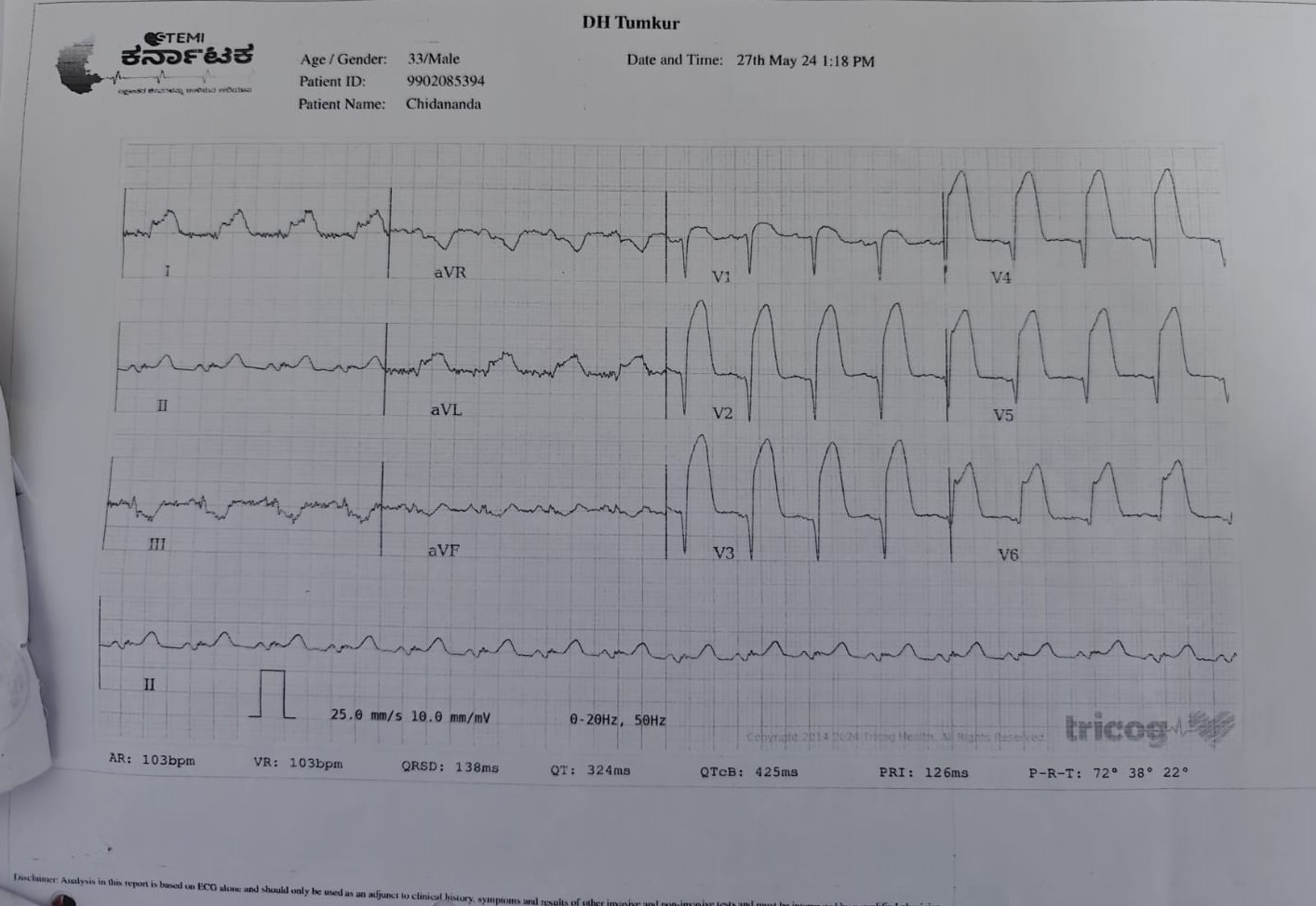
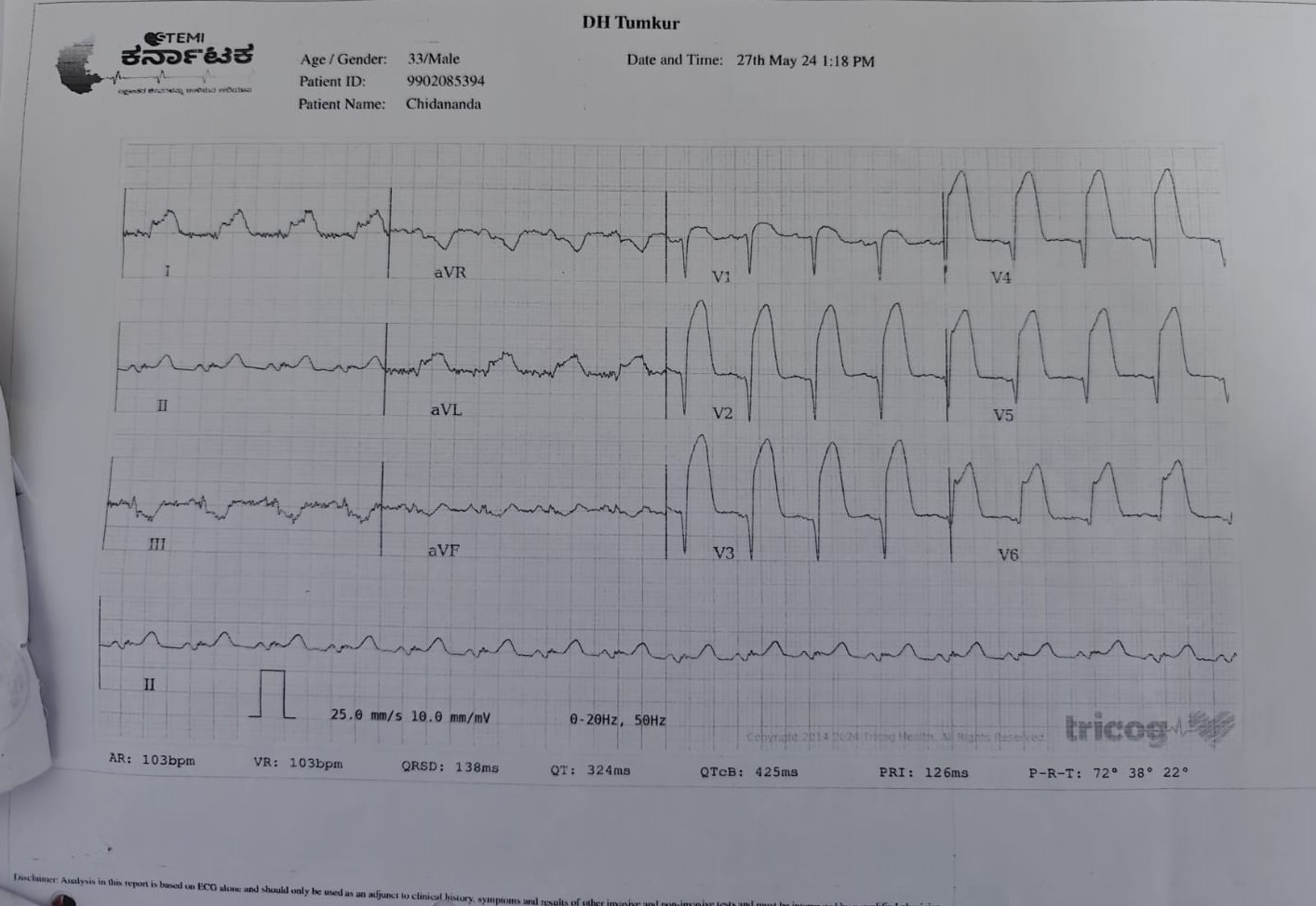
A 33 yrs old gentleman, non diabetic /non hypertensive, a taxi driver by profession, heavy smoker, with family history of CAD (father had undergone PTCA when he was 48yrs) presented to our emergency room with the complaints of acute onset chest pain with profuse sweating for the last 4 hours. On Examination, patient had ongoing chest pain with profuse sweating, BP was low around 84/60mmhg, HR -126/min, O2 sats around 92% in RA, RR was around 22/min. Immediately patient was shifted to CCU.
Relevant Test Results Prior to Catheterization
In ER, Immediately ECG done showed Acute Extensive Anterolateral MI, Bedside echo done showed RWMA +, mid apical anterior, anterolateral akinetic, EF - 35%, mild MR/TR, PASP 50mmhg, IVC partially collapsing. Arterial blood gas analysis showed pH:7.24, pO2:64, pCO2:28, HCO3: 14, Lactate : 6.0
 Chidanand echo 1.avi
Chidanand echo 1.avi
 Chidanand echo 2.avi
Chidanand echo 2.avi
 Chidanand echo 3.avi
Chidanand echo 3.avi
Relevant Catheterization Findings
After informed consent patient taken for emergency coronary angiogram which showed distal LM haziness (? clot) with proximal LAD grade III thrombotic occlusion with distal TIMI II flow. LCx & RCA normal. CAG intepretation was SVD (LM with LAD disease) and plan was to do primary PTCA + stent to LM to LAD. Patient was having ongoing chest pain, had 1 episode of VT (DC cardioverted), increasing breathing difficulty, put on NIV with intubation standby
 Chiddanand 2.mp4
Chiddanand 2.mp4
 Chiddanand 3.mp4
Chiddanand 3.mp4
 Chiddanand 4.mp4
Chiddanand 4.mp4
Interventional Management
Procedural Step
After informed consent patient proceeded for primary PCI through right femoral artery route. 2 Regular workhorse coronary wire taken, 1 parked into distal LCx, other 1 tried crossing the infarct related artery (IRA) but felt some resistance initially and was going towards the lateral side (thought I was in some of the diagonal). We tried balloon dilatation of the ostio-proximal part of IRA with NC balloon 2 X 10mm followed by 2.5 X 10 multiple times but flow in the artery didnt improve.
Viewed CAG in all angles and again tried wiring but couldn't see LAD stump. In the mean time patient continued to have chest pain, another episode of VT (DC cardioverted), BP was dropping further, patient was getting restless.That time lot of things running in my mind, to put IABP support, call colleague/senior for help or take patient back to CCU for IV thrombolysis.
Paused for few seconds and took a closer look at the LAO caudal view and concentrated on LM haziness, maybe LAD stump is arising from the LM i thought, thereafter I took the whisper hydrophilic wire with angulated tip and tried poking the distal LM and succeeded passing the wire. Subsequently balloon dilated with NC 2.5 X 10 and therefore could see the distal LAD, parked the wire in distal LAD, in view of large thrombus with distal slow flow, thrombosuction was done. post thrombosuction, IC NTG & nikoran, flow in LAD improved. Thereafter DES 3.0 X 28mm deployed, post dilated with NC balloon 3 X 15. Good end result.
 Chiddanand 16.mp4
Chiddanand 16.mp4
 Chiddanand 31.mp4
Chiddanand 31.mp4
 Chiddanand 61.mp4
Chiddanand 61.mp4
Viewed CAG in all angles and again tried wiring but couldn't see LAD stump. In the mean time patient continued to have chest pain, another episode of VT (DC cardioverted), BP was dropping further, patient was getting restless.That time lot of things running in my mind, to put IABP support, call colleague/senior for help or take patient back to CCU for IV thrombolysis.
Paused for few seconds and took a closer look at the LAO caudal view and concentrated on LM haziness, maybe LAD stump is arising from the LM i thought, thereafter I took the whisper hydrophilic wire with angulated tip and tried poking the distal LM and succeeded passing the wire. Subsequently balloon dilated with NC 2.5 X 10 and therefore could see the distal LAD, parked the wire in distal LAD, in view of large thrombus with distal slow flow, thrombosuction was done. post thrombosuction, IC NTG & nikoran, flow in LAD improved. Thereafter DES 3.0 X 28mm deployed, post dilated with NC balloon 3 X 15. Good end result.
Case Summary
Post PCI patient was stable, no chest pain, no further VTs noted, No Post MI/PCI complications occured and was discharged in stable condition after 2 days.
Learning points from the case
1. Focused visualisation of CAG from all angles and proper co-relation with ECG and Echo would help2. In this case, thrombus laden Ramus originating along the same angle as LAD created the confusion 33. Staying calm during procedure was important to avoid unfavourable outcomes 4. To know when to stop is important, overdoing may harm5. IVUS/OCT if readily available would have helped to localize LAD ostium early in this case
Learning points from the case
1. Focused visualisation of CAG from all angles and proper co-relation with ECG and Echo would help2. In this case, thrombus laden Ramus originating along the same angle as LAD created the confusion 33. Staying calm during procedure was important to avoid unfavourable outcomes 4. To know when to stop is important, overdoing may harm5. IVUS/OCT if readily available would have helped to localize LAD ostium early in this case
