CASE20240806_006
PCI Nightmares : Confronting the Complications and How to Tackle Them
By Jakkapun Yanyongmathe, Pannipa Suwannasom
Presenter
Jakkapun Yanyongmathe
Authors
Jakkapun Yanyongmathe1, Pannipa Suwannasom1
Affiliation
Faculty of Medicine, Chiang Mai University, Thailand1,
View Study Report
CASE20240806_006
Complication Management - Complication Management
PCI Nightmares : Confronting the Complications and How to Tackle Them
Jakkapun Yanyongmathe1, Pannipa Suwannasom1
Faculty of Medicine, Chiang Mai University, Thailand1,
Clinical Information
Relevant Clinical History and Physical Exam
A 54-year-old male presented with acute de novo heart failure and chest discomfort. He was diagnosed with non-ST elevation myocardial infarction (NSTEMI) and was referred to our hospital for a coronary angiogram.
Relevant Test Results Prior to Catheterization
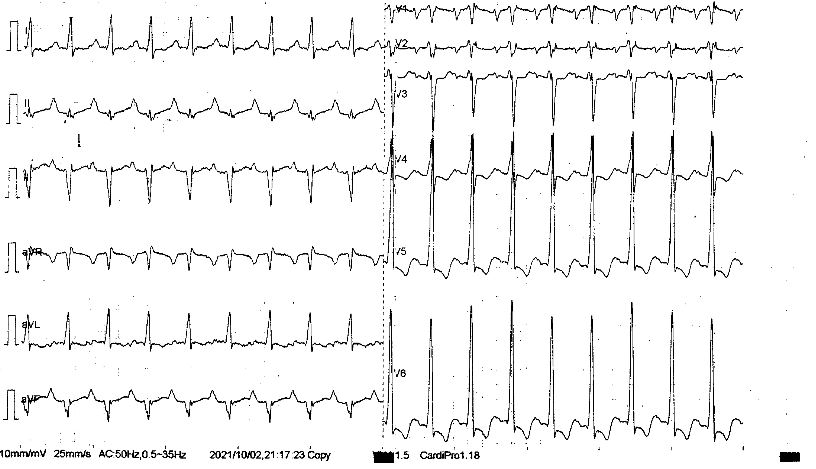
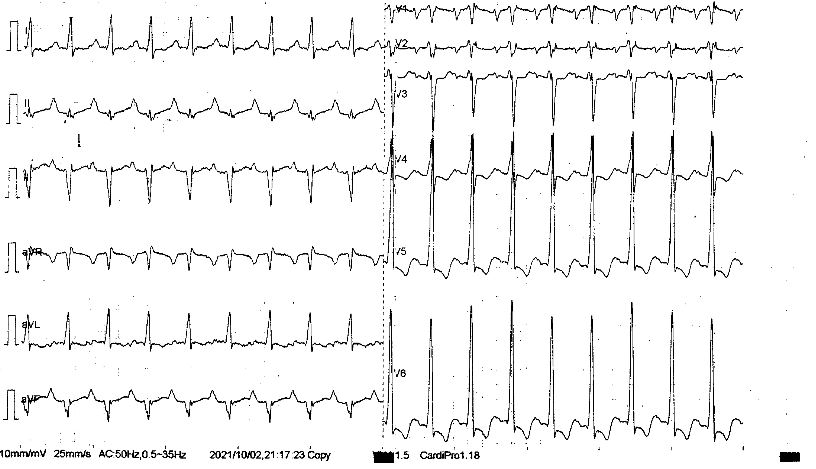
The 12-lead ECG revealed sinus rhythm with complete right bundle branch block (RBBB) and left ventricular hypertrophy with a strain pattern. Laboratory tests showed mild renal impairment (serum creatinine level of 1.4 mg/dL). The echocardiogram demonstrated global hypokinesia and severely impaired left ventricular systolic function, with a left ventricular ejection fraction (LVEF) of 15%.
 Pre PLAX.mp4
Pre PLAX.mp4
 Pre SAX.mp4
Pre SAX.mp4
 Pre A4C.mp4
Pre A4C.mp4
Relevant Catheterization Findings
The coronary angiogram revealed 80% stenosis of the distal left main trifurcation lesion with eccentric calcification, 80% stenosis of the proximal left anterior descending (LAD) artery, and 90% stenosis in the intermediate artery (IM). The right coronary artery (RCA) showed 50% stenosis in the mid-RCA. The heart team has discussed on the mode of revascularization and agreed to proceed for provisional stenting Left main to proximal LAD with the intra-aortic balloon pump (IABP support).
 RCA.mp4
RCA.mp4
 LCA.mp4
LCA.mp4
Interventional Management
Procedural Step
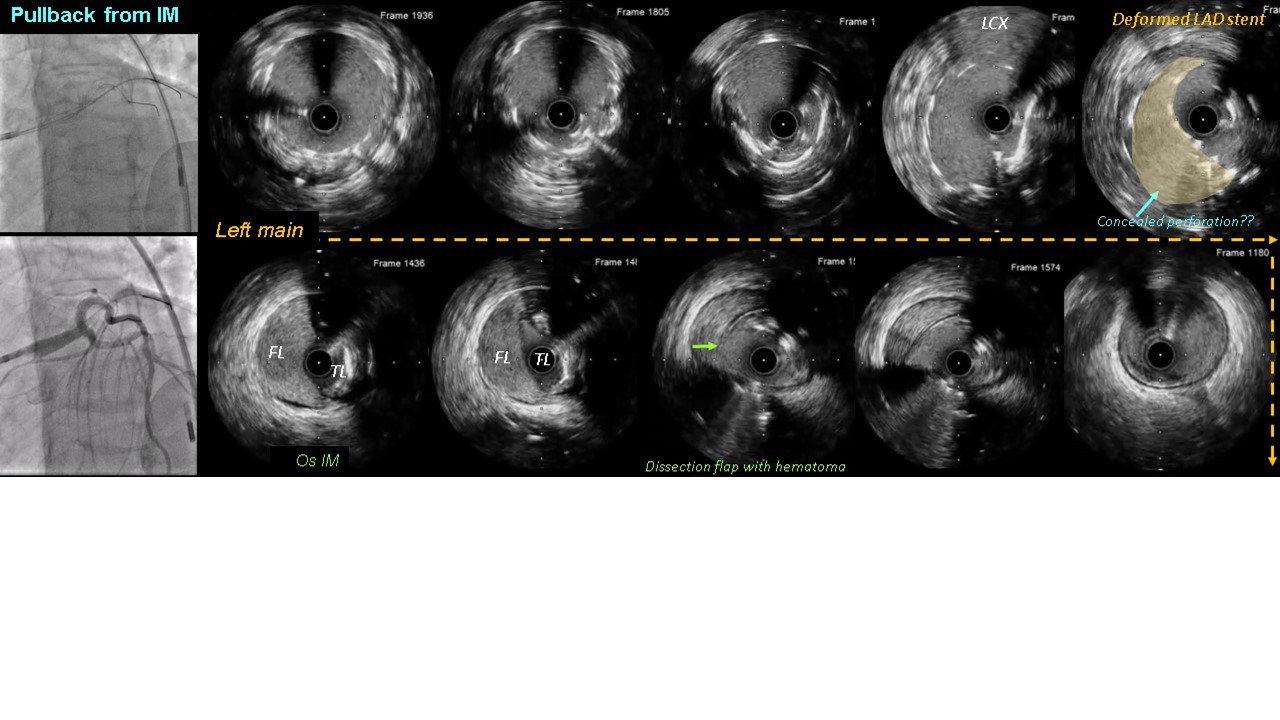
The procedure was performed using 7 Fr guiding catheter. The workhorse guidewires inserted to LAD and intermediate (IM) branch. The IVUS revealed eccentric calcified plaque in LAD and attenuated plaque at distal LM. At that time, the pullback from IM was not performed despite unclear ostial from angiography. A scoring balloon was used for lesion preparation, and a DES were implanted from mid-LM to proximal LAD. After performing POT on the distal LM, the patient developed chest pain. Angiography showed TIMI 1 flow along the IM. We tried to rewire to the IM branch multiple times using the double-lumen catheter but failed. We reviewed the IVUS pullback from LAD and noted that ostial of IM was compromised by the carina shift, thus open the distort carina should be able to return the flow. Consequently, we decided to insert balloon 1.25x10 mm via Sion wire that trapped underneath the LM stent strut. Afterward, the flow via IM was improved. Sequential dilation with 2.0x20 mm was performed and TIMI 3 was achieved. Later, Whisper MS wire was re-inserted from the main branch via double lumen catheter to the ostial of IM. IVUS pullback from the IM confirmed that the wire was in the true lumen with a dissection flap and large hematoma at the ostium of the IM. Subsequently, we performed stenting of the IM using the TAP technique and achieved TIMI flow grade 3 after the final kissing balloon inflation. Six months later, scheduled echocardiogram showed improvement of LVEF from 15% to 40%.
 After POT, IM TIMI 2.mp4
After POT, IM TIMI 2.mp4
 Final CINE.mp4
Final CINE.mp4
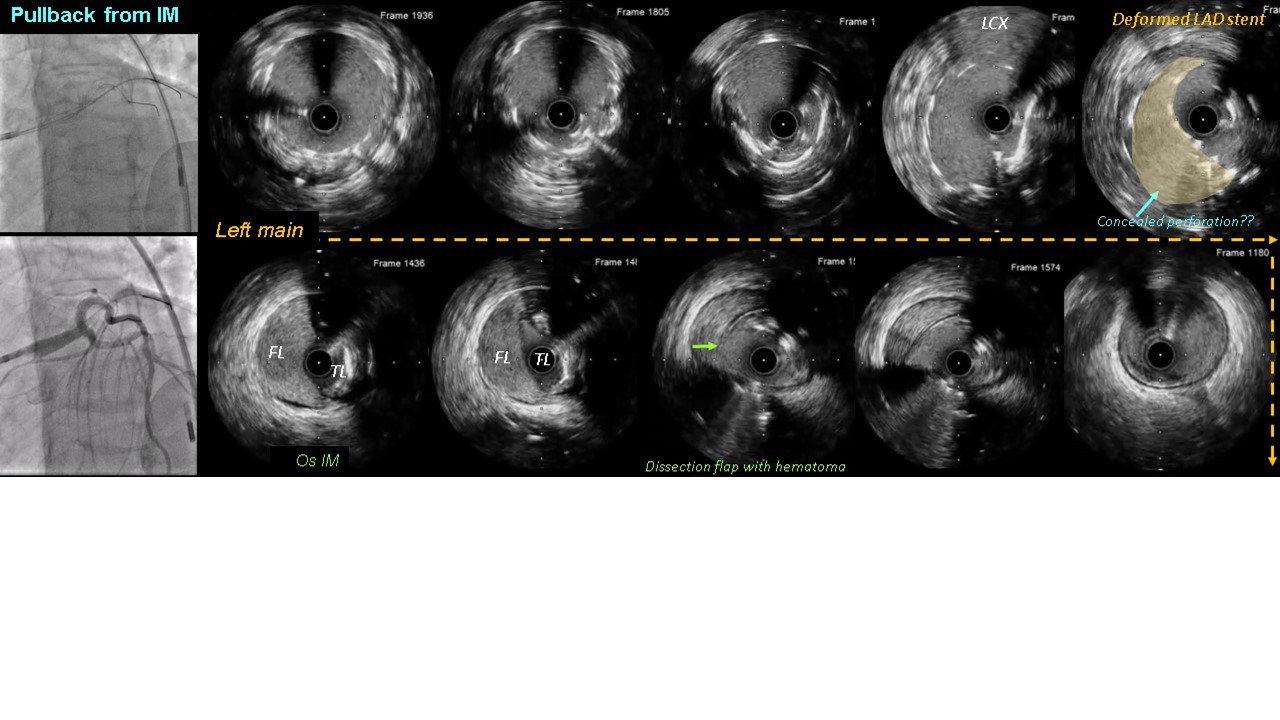
Case Summary
The dissection of the intermediate artery (IM) may have resulted from lesion preparation with a scoring balloon in the left main artery. While deforming the LM strut is generally not recommended, a small balloon was necessary in this case to facilitate wire entry into the IM branch. We emphasize the value of intravascular ultrasound (IVUS) in improving PCI outcomes by confirming wire placement in the true lumen, detecting complications, and optimizing stenting.
