CASE20240806_005
The Nightmare Case of Twice Leakage
By Poh Chanyavanich, Wiwat Kanjanarutjawiwat
Presenter
Poh Chanyavanich
Authors
Poh Chanyavanich1, Wiwat Kanjanarutjawiwat1
Affiliation
Phrapokklao Hospital, Thailand1,
View Study Report
CASE20240806_005
Complication Management - Complication Management
The Nightmare Case of Twice Leakage
Poh Chanyavanich1, Wiwat Kanjanarutjawiwat1
Phrapokklao Hospital, Thailand1,
Clinical Information
Relevant Clinical History and Physical Exam
A 75-year old female presented with recurrent resting chest pain radiated to shoulders for 3 days. Her coronary risk factors were hypertension and hypercholesterolemia.Physical examination showed blood pressure 163/102 mmHg, pulse rate 60 beat/min, normal S1S2, no murmur, normal breath sound, no pitting edema.Initial diagnosis was NSTE-ACS with Grace risk score of 131, she was referred for coronary angiography.
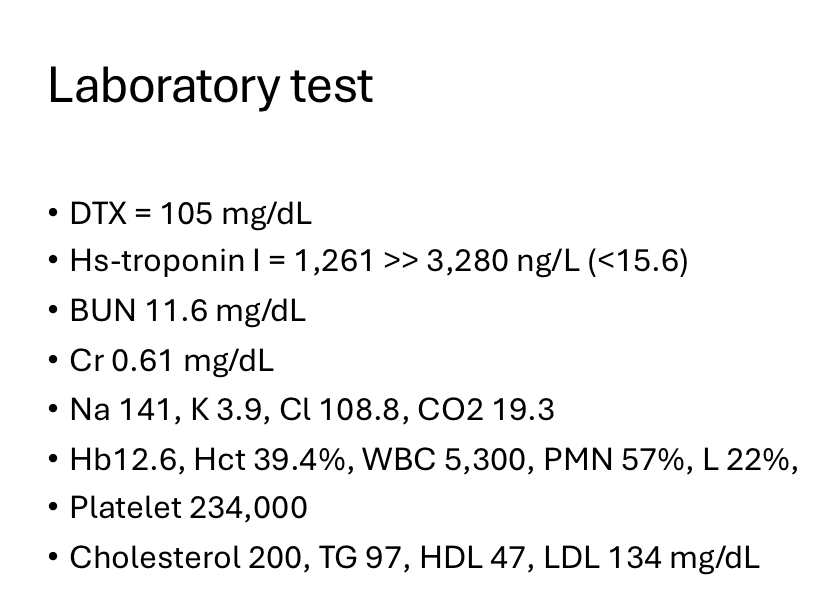
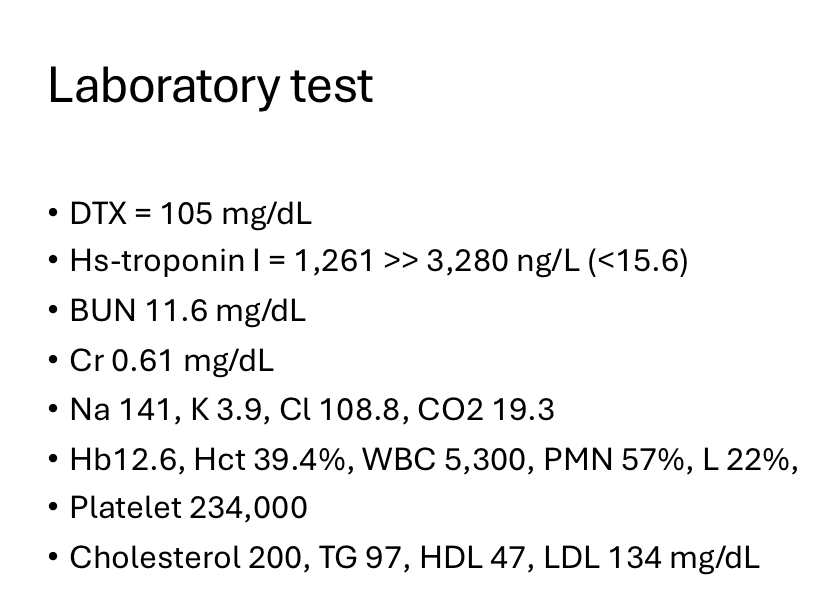
Relevant Test Results Prior to Catheterization
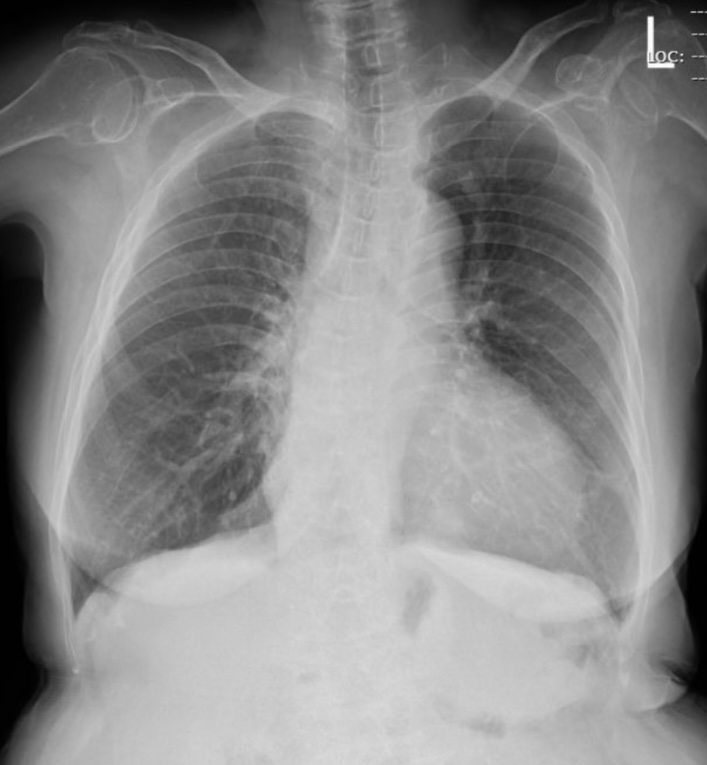
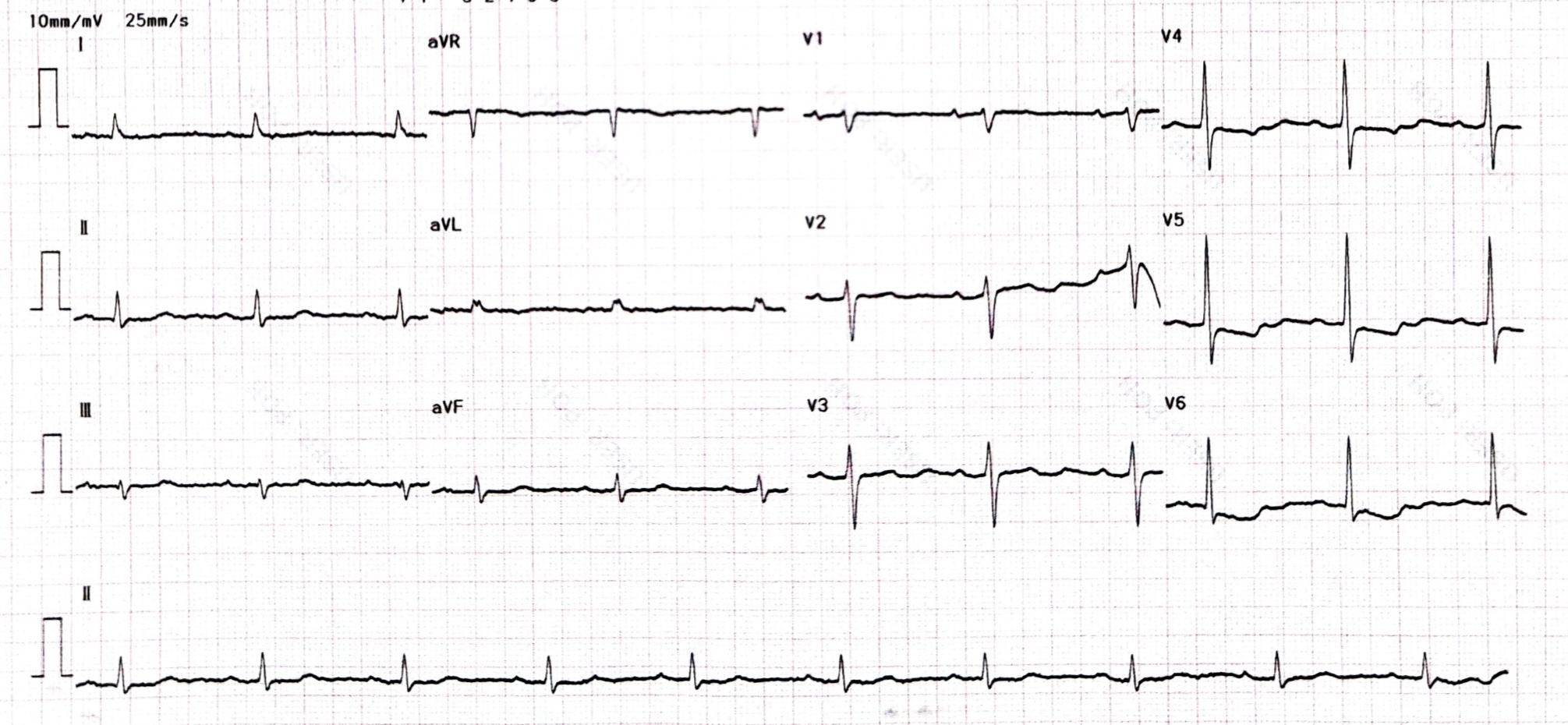
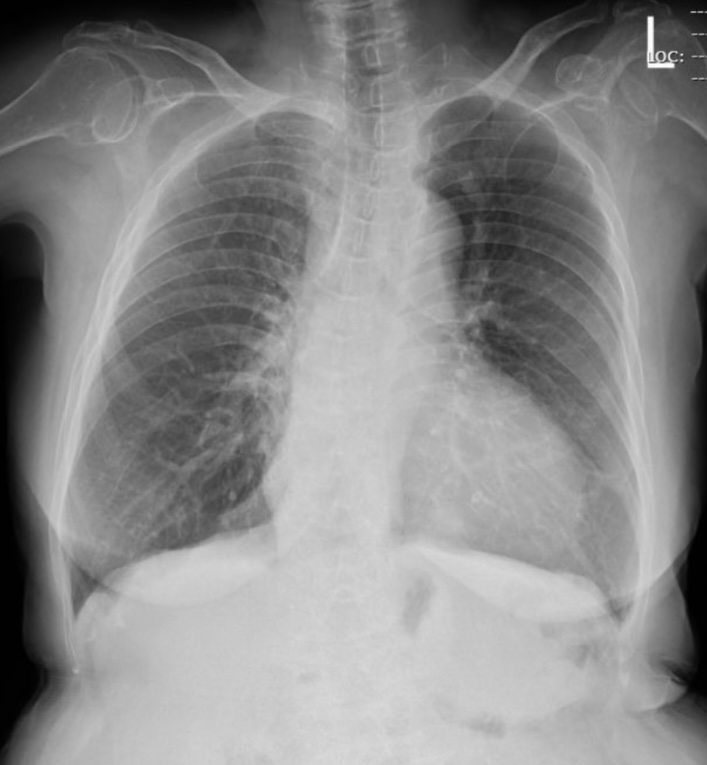
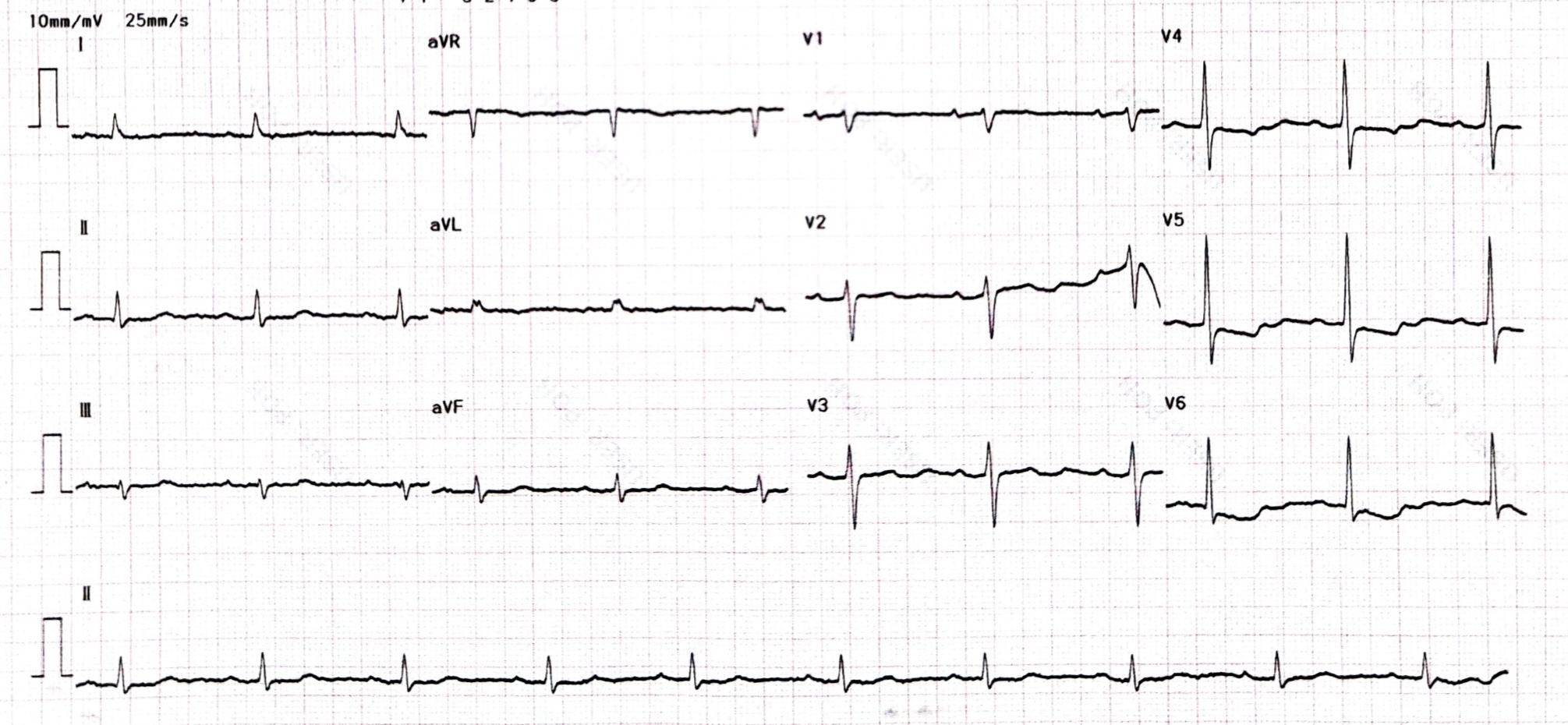
- EKG showed normal sinus rhythm with down slope ST depression at V4-6.- CXR showed Cardiomegaly, no pulmonary congestion. Laboratory test- Troponin I 1,261 >> 3,280 ng/L (normal < 15.6 ng/L)Echocardiography- Concentric LVH, LVEF 57%, inferior wall hypokinesia from mid to apex- Diastolic dysfunction grade 1- Mild MR, TR- No pericardial efffusion
Relevant Catheterization Findings
Coronary angiogram showed triple vessels disease with heavy calcified left main and LAD. Due to high SYNTAX score (score = 45), patient was sent to discuss with cardiothoracic surgeon but she and her family denied CABG (STS operative mortality 3%). They preferred PCI as a mode of revascularization, we performed PCI at RCA with DES then staged PCI at left main and LAD with rotational atherectomy.
 Movie_Lateral(2).mp4
Movie_Lateral(2).mp4
 Movie_Frontal(5).mp4
Movie_Frontal(5).mp4
 Movie_Frontal(4).mp4
Movie_Frontal(4).mp4
Interventional Management
Procedural Step
- Femoral access with guiding JL 3.5 7 Fr, Rota floppy wire.
 Movie_Frontal(11).mp4
Movie_Frontal(11).mp4
 Movie_Frontal(32).mp4
Movie_Frontal(32).mp4
 Movie_Frontal(62).mp4
Movie_Frontal(62).mp4
- Rotational atherectomy with Rota Burr 1.5, 160,000 rpm for 3 runs, at left main to proximal LAD.
- IVUS showed 270 degree calcified proximal LAD with severe hematoma at proximal LAD.
- PCI with DES 2.25 x 24 mm at mid LAD then PCI LM-LAD with DES 3.0 x 30 mm.
- Severe chest pain and hypotension after deployed stent at LM-LAD, coronary angiogram showed severe coronary perforation, Ellis grade III.
- We used balloon stent prolong inflation then inserted guide extension and PCI with covered stent 2.5x20 mm at perforation site. Diagonal was lossed after covered stent placement.
- Patient had cardiac arrest, we started CPR, intubation, pericardiocentesis and autotransfusion.
- POT LM with NC balloon 3.5 x 8 mm. IVUS showed good stent expansion, no distal edge dissection.
- We inserted IABP to maintain coronary perfusion and support hemodynamic.
- Hemodynamic was stable and patient was transferred to CCU.
- After 2 hour at CCU, patient had cardiac arrest with evidence of 400 ml hemopericardium, we start autotransfusion during CPR and emergency transferred patient to cathlab.
- Angiogram showed re-perforation at proximal LAD, we balloon with NC balloon 3.0x12 mm at proximal LAD.
- After observed at cathlab without rebleeding, we gave Protamine 50 mg intravenous due to prolong ACT.
- Patient hemodynamic was stable and gradually improved.
Case Summary
This is an Ellis coronary perforation type III, starting with coronary hematoma after rotational atherectomy. This may be prevented by initial used imaging and selected smaller rota burr because the vessel had negative remodeling. After sealed the perforation with covered stent, there was stent malapposition (reviewed IVUS), this would explained the mechanism of rebleeding at the perforation site.
Careful evaluation of imaging pre and post procedure can prevent complication in complex PCI procedure.
This case had length of stay in hospital for 10 days. Angiogram before discharge showed patent LAD and RCA gave collateral to DG.
Patient can visit at OPD with good functional status at 3 months.
