CASE20240721_002
Challenging Access and Procedure: Distal Transradial RotaTripsy Percutaneous Coronary Intervention to Coronary Nodular Calcification
By Han Bing Chow
Presenter
Han Bing Chow
Authors
Han Bing Chow1
Affiliation
Tuen Mun Hospital, Hong Kong, China1,
View Study Report
CASE20240721_002
Complex PCI - Calcified Lesion
Challenging Access and Procedure: Distal Transradial RotaTripsy Percutaneous Coronary Intervention to Coronary Nodular Calcification
Han Bing Chow1
Tuen Mun Hospital, Hong Kong, China1,
Clinical Information
Relevant Clinical History and Physical Exam
We report an 80-year-old gentleman with history of hypertension, obstructive sleep apnoea, hypothyroidism, hypercholesterolemia, diabetes mellitus and gout. Following stable angina symptoms which has persisted for a year, he underwent a computed tomography coronary angiography (CTCA) examination which revealed a calcium score of 3531.


Relevant Test Results Prior to Catheterization
Echocardiogram showed
Relevant Catheterization Findings
TRAP 5Fr diagnostic catheter
Interventional Management
Procedural Step
Unsuccessful attempt in introduction of long sheath through right femoral access (attempt with Terumo 7Fr Destination sheath and Silverway/ Advantage guidewire) due to severe calcification and tortuosity; and introduction of guiding catheter through right radial access (attempt with SAL 0.75 7Fr, ExpressMan guide extension, Advantage guidewire) due to subclavian vessel tortuosity. Successful engagement of right system with distal left radial approach with SAL 0.75 7Fr. Rotational atherectomy was performed with 1.5mm RotaPro for 2 runs at 180,000 rpm. Procedure was complicated with ventricular standstill but self-limited. Optical Coherent Tomography (OCT) performed with Dragonfly Opstar showed diffuse calcification with an eruptive calcium nodule at mRCA. We then opted to perform intravascular lithotripsy with Shockwave 3.5/12 balloon. A total of 20 shocks was performed but was complicated with ruptured balloon (no significant dissection/perforation). Lesion was further prepared with NSE Aperta 3.0/13.Another attempt of intravascular lithotripsy was performed with Shockwave 3.5/12 balloon up to 60 shocks, after which good expansion of balloon was achieved. Lesion was then further prepared with NC Trek Neo 3.5/15 before deploying Xcience Skypoint 3.5/48 overlapped with Xcience Skypoint 4.0/8. Stent was optimized with high pressure NC balloons under OCT guidance. Final angiography results were satisfactory. Medical therapy was planned for the left coronary lesions.
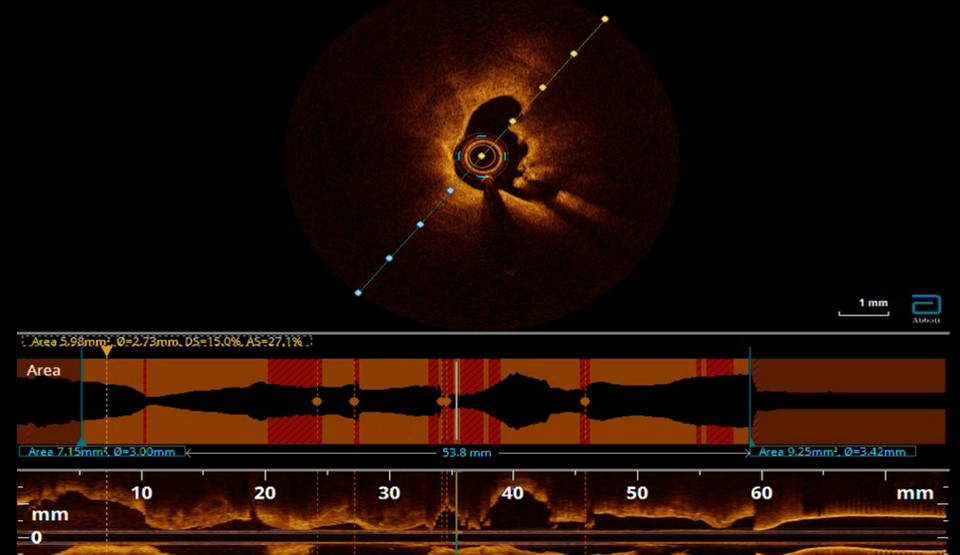

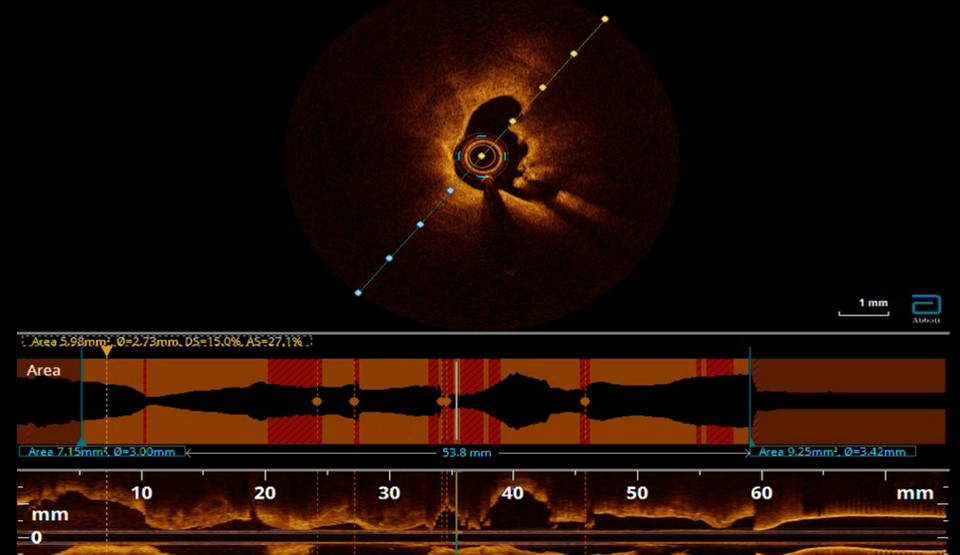

Case Summary
During the intervention of severe calcification and calcium nodule, a standalone calcium modification technique might be inadequate in the angioplasty of the lesion. In the absence of adequate calcium modification, more aggressive combinations of calcium modification should be performed prior to drug eluting stent (DES)/drug eluting balloon (DEB) deployment. Moreover, intravascular imaging is invaluable in coronary calcium assessment, treatment planning and evaluation of stent outcome. We demonstrated the importance of pre-procedural planning and feasibility of RotaShock in debulking and preparation of a massive coronary calcium nodule.
