[COMPLEX PCI] Guideline and concept changes: revascularization for Left Main in 2022
End of zero-sum game in Left Main disease? More support for CABG and PCI being complementary approaches, putting patient preference at heart of decision-making
 Percutaneous coronary intervention (PCI) may not lower mortality risk more than bypass surgery in left main (LM) – a leading interventional cardiologist said – but both are complementary strategies for achieving different clinical endpoints, making patient preference important.
Percutaneous coronary intervention (PCI) may not lower mortality risk more than bypass surgery in left main (LM) – a leading interventional cardiologist said – but both are complementary strategies for achieving different clinical endpoints, making patient preference important.
“Evidence generated so far makes it safe to say that PCI does not improve survival more than coronary artery bypass grafting (CABG) in patients with stable ischemic heart disease (SIHD),” Duk-Woo Park, MD, PhD(Asan Medical Center, Seoul, South Korea) said at COMPLEX PCI 2022 on Nov 24 at the Grand Walkerhill Seoul in South Korea.

Duk-woo Park, MD, PhD presents evolving concepts and guideline recommendations on revascularization for LM disease at the COMPLEX PCI 2022 conference held at the Grand Walkerhill Seoul in South Korea on Nov 24.
“However, PCI plays a key role in acute coronary syndrome (ACS), especially for improving patient-oriented outcomes of angina patients who are either unresponsive to medical therapy, unwilling to take anti-anginal medication or unwilling to undergo invasive CABG,” he said.
Although tradition held CABG as the gold standard of treatment for a wide spectrum of SIHD patients, especially those with LM-coronary artery disease (CAD), technological and technical advancements in PCI and optimal medical therapy (OMT) spurred requests to replace “outdated” studies that cast PCI in an unfavorable light against OMT and CABG.
As an interventional cardiologist, the evidence generated so far makes it safe to say that PCI does not improve survival more than CABG in SIHD.
Both older and more recent studies on SIHD – including MASS II (2004), COURAGE (2007), BARI 2D (2009) and FAME-2 (2012) – had shown negative or neutral results with PCI compared to OMT for the “hard” clinical endpoints of all-cause or cardiovascular (CVD) mortality.
Studies on multivessel disease (MVD) – including the SYNTAX (2019), BEST (2015), FREEDOM (2012) and FAME-3 (2022) trials – also found lower rates of major adverse cardiovascular events (MACE) with CABG compared to PCI.
However, contemporary studies incorporating state-of-the-art PCI – including SYNTAX-LM (2010), PRECOMBAT (2011) and EXCEL (2016) – began demonstrating comparable outcomes between stenting and surgery, reporting no statistically significant difference between PCI and CABG for all-cause mortality and the primary endpoint.
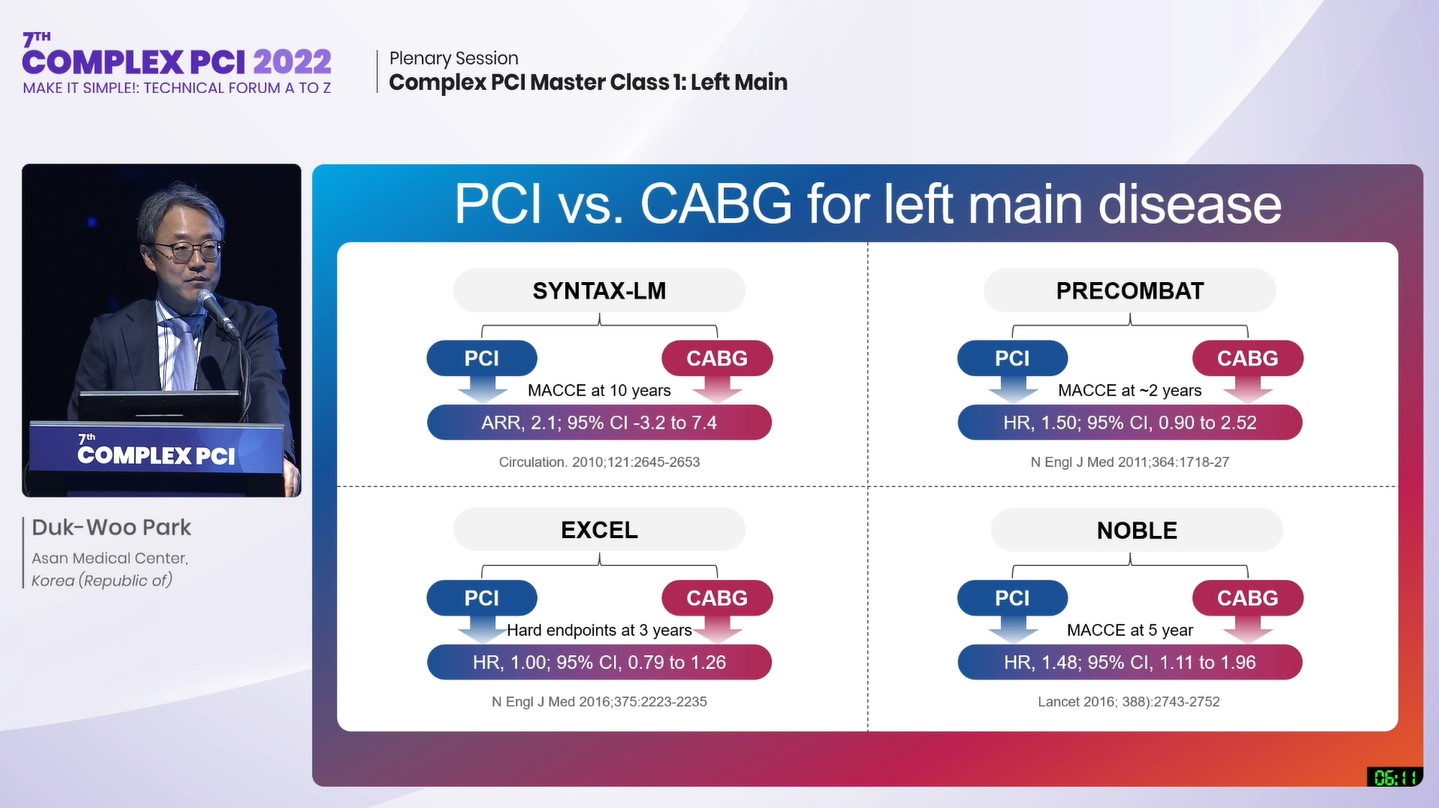
Studies on state-of-the-art PCI versus CABG in LM disease.
Source: Duk-woo Park slides at COMPLEX PCI 2022
Notably, the 10-year follow-up results for mortality from SYNTAX-LM(CABG 26.7% vs. PCI 26.1%; HR 0.90; 95% CI; 0.68-1.20; P=0.47) and AMC’s 10-year PRECOMBAT LM (CABG 13.8% vs. PCI 14.5%; HR 1.13; 95% CI; 0.75-1.70; P=0.57) further signaled comparability between strategies.
The 5-year follow-up of the EXCEL trial, which reported comparable outcomes between bypass surgery and PCI for major adverse cardiac and cerebrovascular events (MACCE), infamously came under fire for controversial interpretations of outcomes and fueled the debate between cardiac surgeons and interventionalists.
Along with significant study limitations of the EXCEL trial – including underpowered outcomes (“prone to false negatives”), no adjustment for multiplicity (“prone to false positives”) and no P-values (“not designed for hypothesis testing”) –other contemporary studies, like the REVIVED-BCIS2 study also found no survival benefit with PCI over OMT, raising calls for more concrete data.
PCI plays a key role in ACS by improving patient-oriented outcomes of angina patients who are either unresponsive to medical therapy, unwilling to take anti-anginal medication or unwilling to undergo invasive CABG.
Interventional cardiologists tended to call for new randomized trials with “different patients, better stents, more IVUS or FFR, more follow-up or other trial endpoints” any time a new series of trials reported neutral or worse outcomes with PCI compared to OMT or CABG, Park explained, despite the lack of mortality benefit with PCI: “The higher benefit of survival with CABG over PCI was a key issue in many (observational) studies like EXCEL and urged individual patient data (IPD) meta-analysis.”
The highly anticipated meta-analysis – published in the Lancet last year by Marc S. Sabatine, MD (Brigham and Women's Hospital, Boston, USA) and investigators, including ones at AMC – found no significant difference in all-cause mortality between treatment arms (PCI 11.2% vs. CABG 10.2%; HR 1.10; 0.91-1.32; P=0.33), indicating a statistically non-significant absolute difference of 0.9% (-0.9-2.8).
Outcomes of the meta-analysis, which encompassed the four major trials of SYNTAX Left Main, PRECOMBAT, NOBLE and EXCEL, also found no significant difference between PCI and CABG arms after adjusting for SYNTAX scores (HR 1.09; 0.91-1.31).
Separate analysis of the SYNTAX and PRECOMBAT studies, both with follow-up to 10-years, demonstrated no significant between-group differences for the endpoint of all-cause mortality (CABG 22.1% vs. PCI 21.6%; HR 0.96; 0.76-1.21; P=0.72).
The major finding, Park said, was no difference for the primary outcome of all-cause mortality between PCI and CABG for LM patients at intermediate- or low-anatomic risk but each approach had tradeoffs: CABG with higher risks for stroke (CABG 3.1% vs. PCI 2.7%; HR 0.84; 0.59-1.21; P=0.36) and procedural MI (4.7% vs. 3.2%; HR 0.67; 0.48-0.93; P=0.015); PCI had higher rates of spontaneous MI (2.6% vs. 6.2%; HR 2.36; 1.71-3.23; P<0.0001).
“PCI with drug-eluting stents (DES) and CABG were deemed equally suitable revascularization approaches for LMCAD patients with a median SYNTAX score of 25,” Park said. “CABG had fewer spontaneous MIs and repeat revascularizations and PCI had lower rates of early stroke and procedural MI, although procedural MI rates depended on the definitions used.”
Based on findings from EXCEL and the more recent ISCHEMIA study, big changes are expected for upcoming guidelines for coronary artery revascularization, he said, especially for LMCAD patients.
The takeaway is that contemporary evidence proves comparable outcomes between PCI and CABG for hard clinical endpoints.
The 2021 American College of Cardiology, American Heart Association and Society for Cardiovascular Angiography and Interventions (ACC/AHA/SCAI) guidelines for LMCAD strongly recommended CABG for patients with SIHD and significant LM stenosis to improve survival (Class 1; B-R).
For PCI, the American guidance gave a weaker Class 2a (B-NR) recommendation in selected patients with SIHD and significant LM stenosis for whom PCI can provide similar revascularization of CABG as a “reasonable” option to improve survival.
The latest 2018 European Society of Cardiology and European Association for Cardio-Thoracic Surgery (ESC/EACTS) guidelines for LMCAD strongly recommended only CABG for a wide spectrum of patients with LM disease irrespective of SYNTAX scores (Class I; A).
For PCI, the European guidance, “issued before the REVIVED-BCIS2 and ISCHEMIA studies,” strongly recommended PCI only for LM patients with low SYNTAX scores from 0-22 (Class I; A), gave a Class IIa (A) recommendation for LM patients with intermediate SYNTAX scores (23-32) and contraindicated PCI for high SYNTAX scores ≥33 (Class III; B).
Along with anticipated guideline updates, more studies on the long-term treatment effects of CABG versus state-of-the-art PCI, specifically in groups like diabetes, heart failure with reduced ejection fraction (HFrEF) and distal LM bifurcation disease, could help improve outcomes, Park said.
A state-of-the-art review on the evolution and updated management of LM disease, published Apr 2 by Sang-woo Park, MD and AMC investigators in JACC: Asia, noted that more data on “reasonable” incomplete revascularization, optimal stent strategy for distal LM bifurcation disease and optimal antithrombotic strategy after complex PCI (particularly for Asian patients) could help resolve conflicting issues.
The patient should be at the center of the decision-making process along with the expertise of the interventionalist and surgeon and resources of the medical institution.
Another state-of-the-art review published by Paul W. Armstrong, MD (University of Alberta, Edmonton, Canada) and colleagues in the European Heart Journal on Sept 29 named factors that favored each treatment pathway to help decision-making between modalities for SIHD patients.
| Treatment pathways for SIHD patients | ||
|---|---|---|
| Favors OMT | Favors PCI | Favors CABG |
| - Minimal symptoms - Good quality of life - Tolerates medical therapy and reaches target goals - Adheres to careful follow-up - Patient preference |
- High surgical risk - Low-complexity plaques - Low-quality CABG conduits - Elderly patients with serious comorbidities - Preference for fast recovery |
- Diabetes - Complex MVD - Moderate/severe LV dysfunction - Requires concomitant cardiac surgery - Long-term survival |
| Source: Paul W. Armstrong et al. Left main coronary disease: evolving management concepts published in the European Heart Journal, Volume 43, Issue 44, 21 November 2022, Pages 4635–4643, https://doi.org/10.1093/eurheartj/ehac542 | ||
Along with the anatomical and physiological characteristics of the patient, factors such as the volume, expertise and experience of the interventionalist, cardiac surgeon and medical institution were also important factors.
“Through shared decision-making, these comprehensive factors should help inform the individual patient of the optimal treatment choice for LM disease,” Park said. “The takeaway is that contemporary evidence proves comparable outcomes between PCI and CABG for hard clinical endpoints.”
“PCI and CABG are different interventions performed with different patients by different physicians with different aims,” he said. “The patient should be at the center of the decision-making process with the heart team – these two central elements are joined across an axis that integrates the expertise of the interventionalist and surgeon, along with the resources and characteristics of the medical institution.”
Edited by

Duk-Woo Park, MD
Asan Medical Center, Korea (Republic of)
Written by

YoonJee Marian Chu, Medical Journalist
Read BiographyPark reported grants from Daiichi Sankyo, ChongKunDang Pharm, and Daewoong Pharm; personal fees from Edwards and Medtronic; grants and personal fees from Abbott Vascular.
