CASE20220823_001
When It Rains It Pours: Having Two Complications At The Same Time
By
Presenter
Hsuan-Ling Tseng
Authors
1
Affiliation
, Taiwan1
Complications - Complications
When It Rains It Pours: Having Two Complications At The Same Time
1
, Taiwan1
Clinical Information
Patient initials or Identifier Number
CTL
Relevant Clinical History and Physical Exam
A 83 year-old man with a history of hypertension and hyperlipidemia presented with intermittent chest tightness to our cardiology clinic. He also complained of dyspnea on exertion. He denied history of smoking. Physical exam showed bilateral clear breathing sound, regular heart beat without cardiac murmur and no pitting edema.
Relevant Test Results Prior to Catheterization
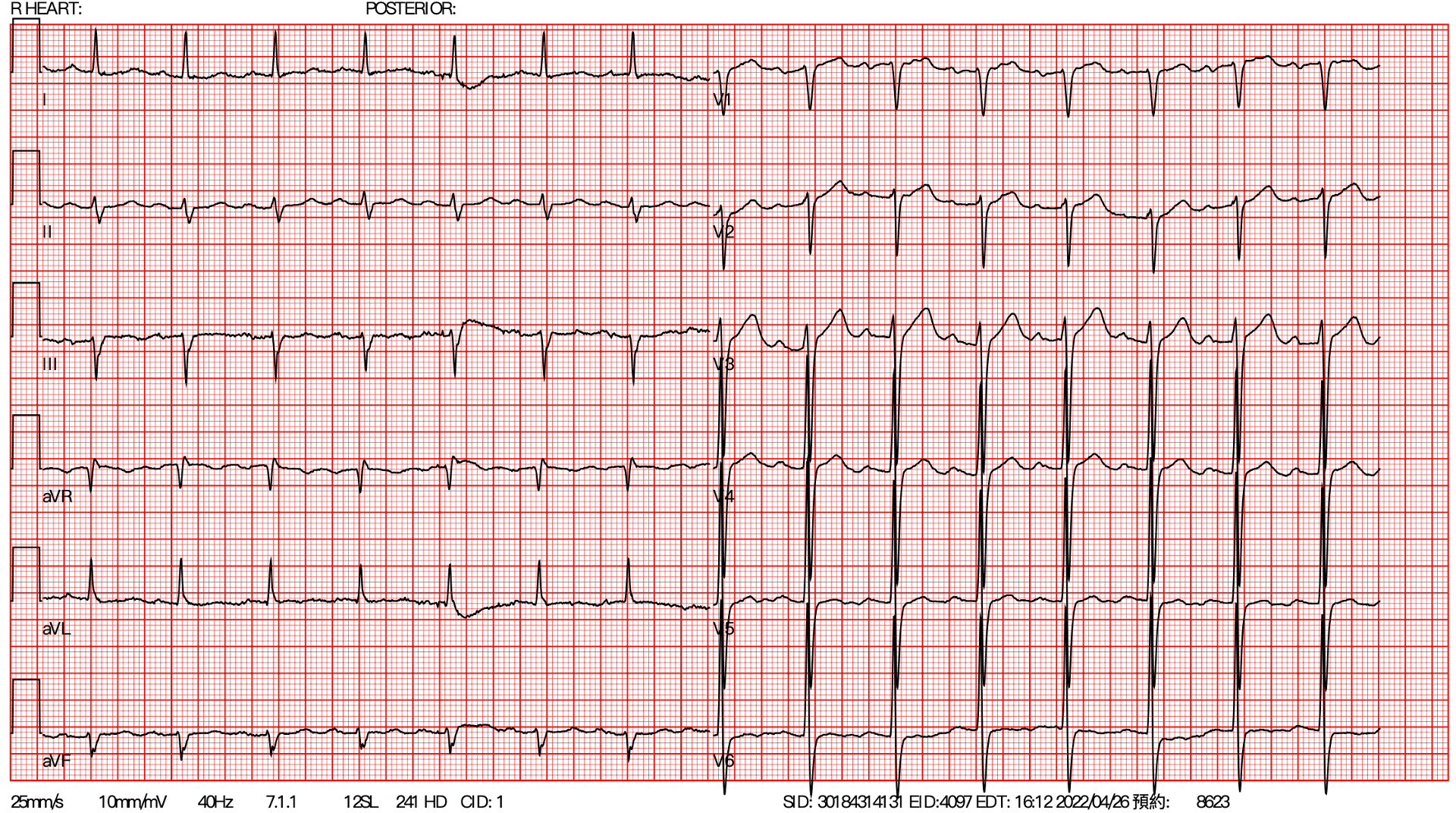
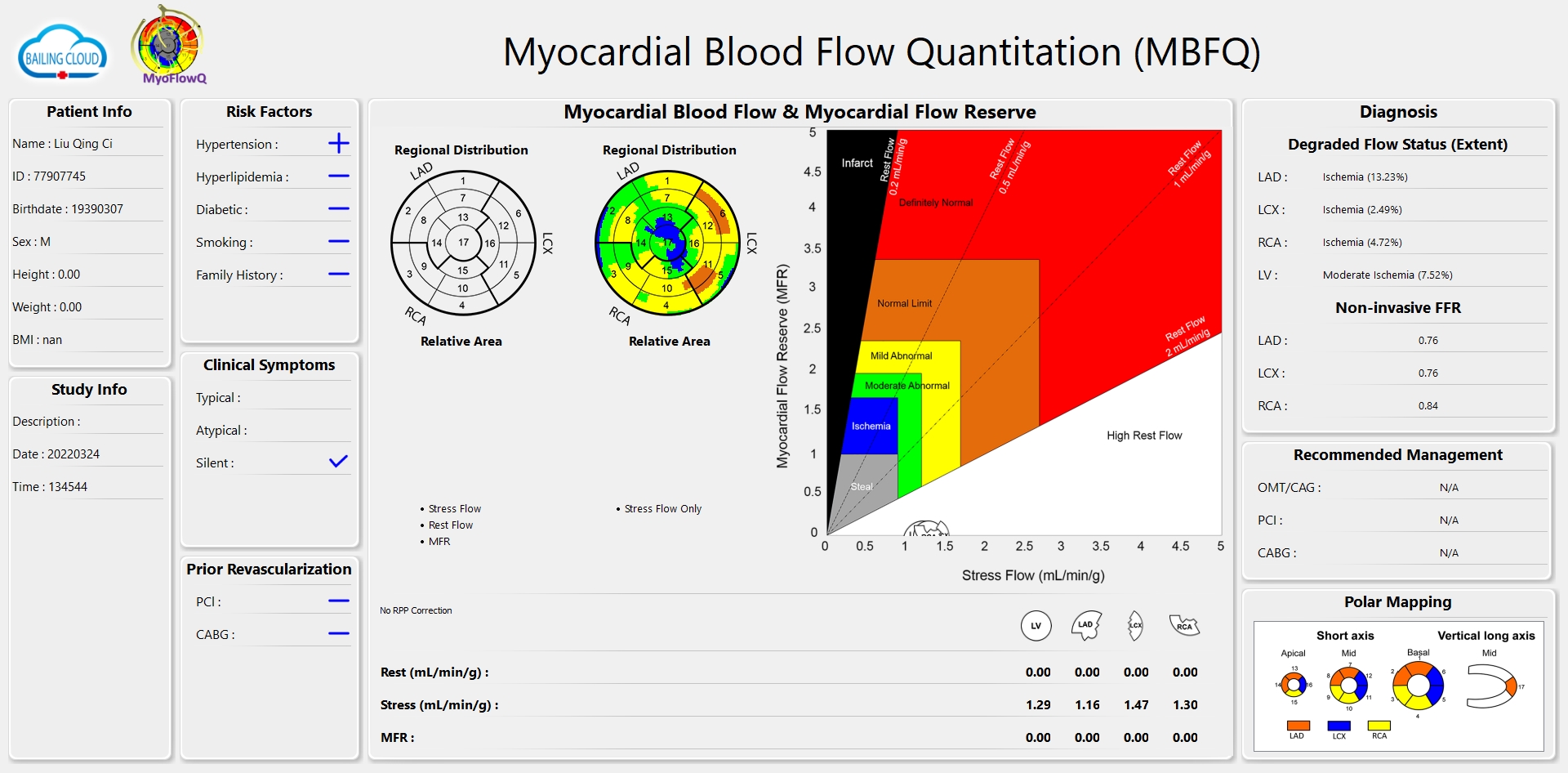
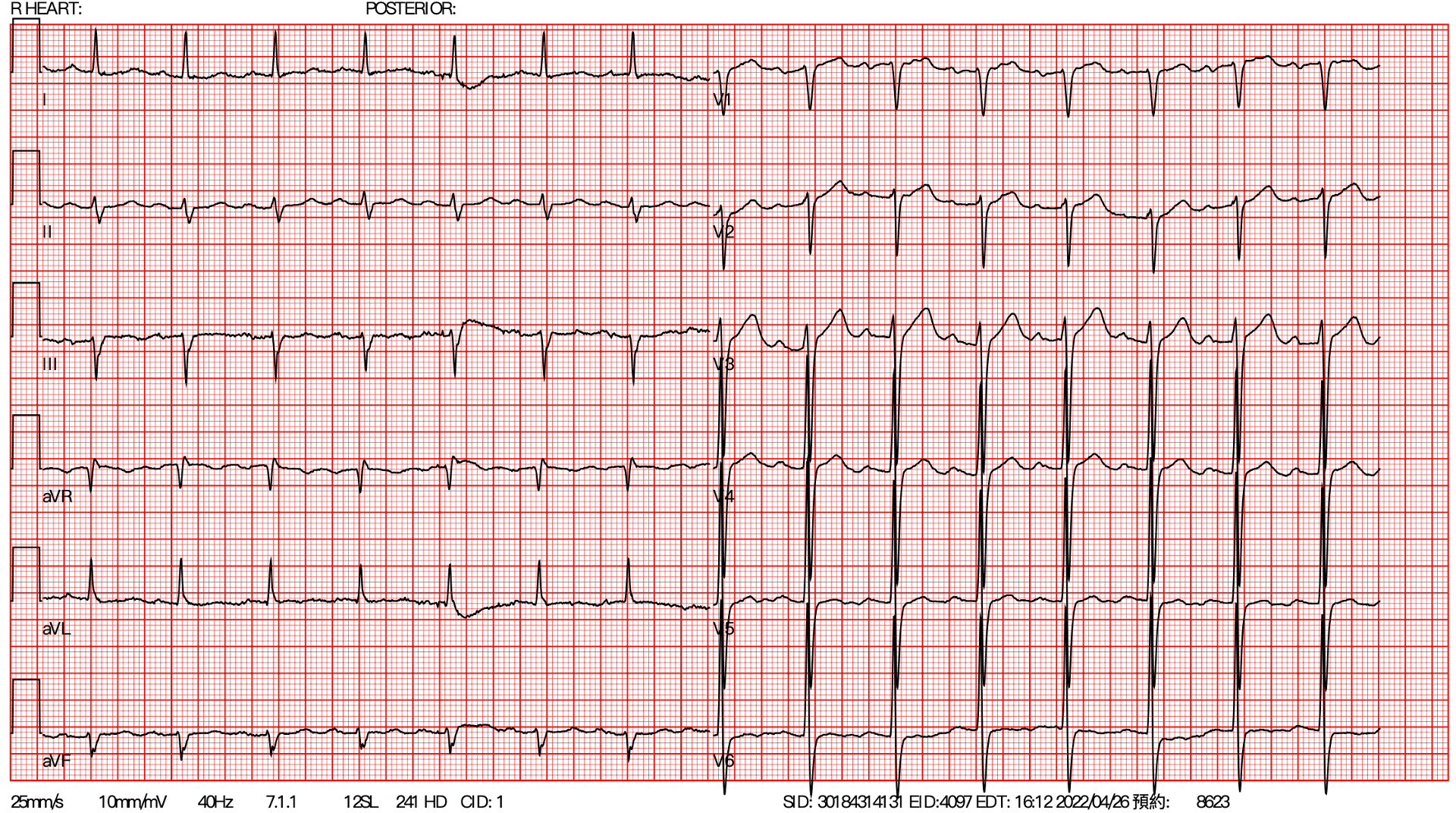
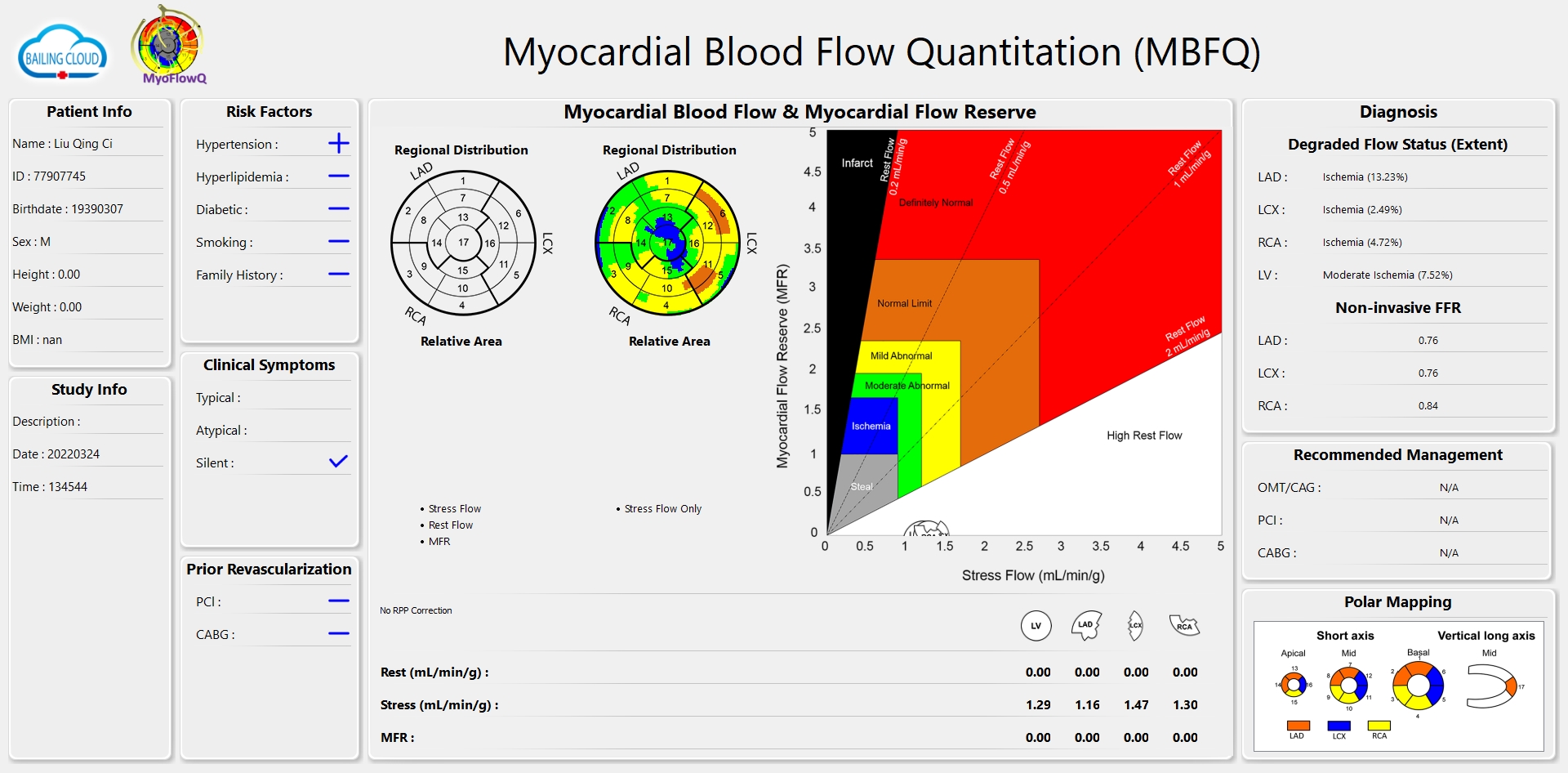
ECG showed no ischemic change. Myocardial perfusion scan showed moderate ischemia of left ventricle.
Relevant Catheterization Findings
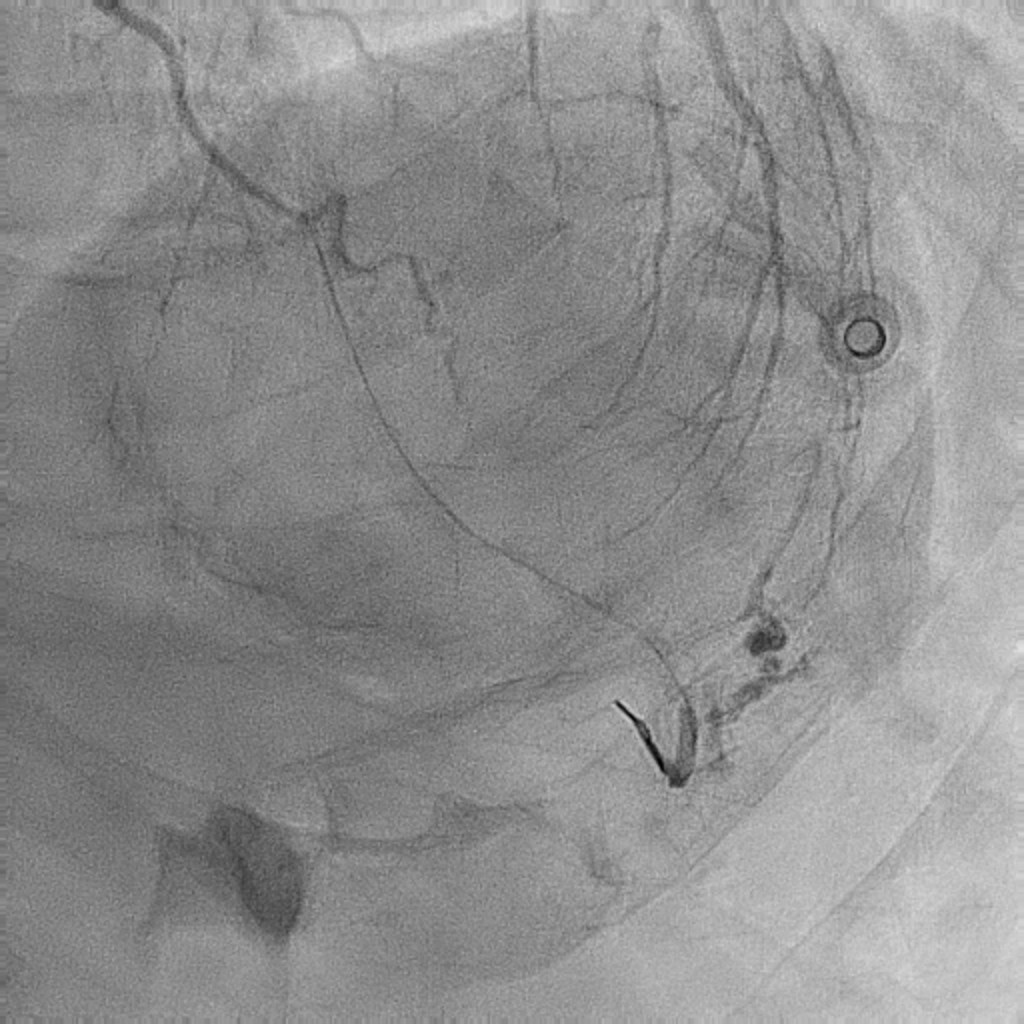
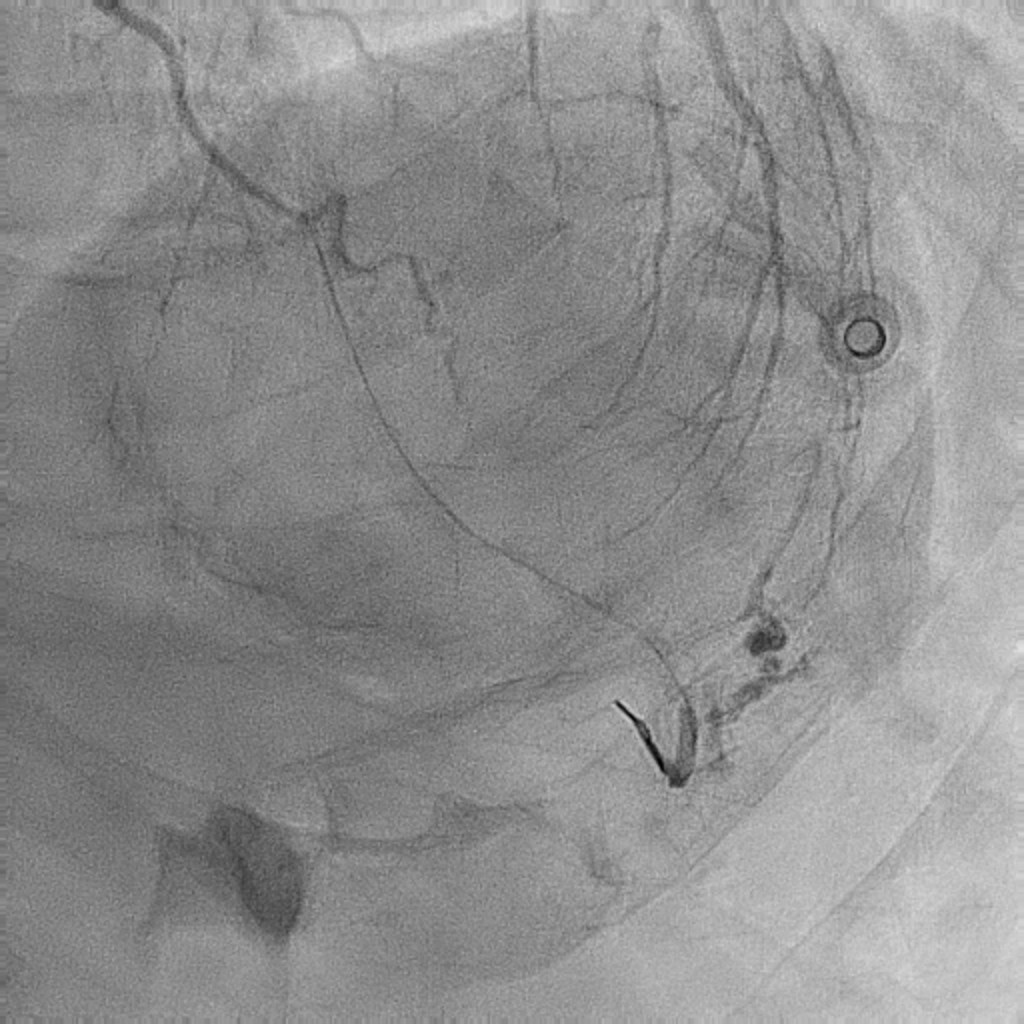
LAD: diffuse stenosis from proximal to distal partLCX: stenosis at proximal and distal part, ostial stenosis of OM branchRCA: very tortuous, tandem lesion at proximal and middle partCAD, 3-V-D, syntax score above 33
 1.mp4
1.mp4
 2.mp4
2.mp4
 3.mp4
3.mp4
 5.mp4
5.mp4
 6.mp4
6.mp4
 7.mp4
7.mp4
Interventional Management
Procedural Step
At first, we consulted heart team and discussed with the patient and his family about CABG. However, they refused surgical treatment due to old age. Our strategy was complete revascularization and fix LCX and LAD this time. We used 6Fr EBU 3.5 as guiding catheter and runthrough as workhorse wire. A NC balloon was used for pre-dilatation for LCX lesion. A DES was placed from OM to proximal part. Another DES was placed at proximal part. We used NC balloon for post-dilatation. Something wrong at OM but we didn't notice. Then we start to fix LAD lesion but extravasation was noted at OM distal. Due to distal perforation, we went back to OM and used prolong ballon inflation for 5 minutes several times to fix it. Hemodynamic change was noted but echocardiography showed no pericardial effusion. However, another extravasation at ostium of the branch of OM. Type C dissection was favored and we observed it. We went back to LAD and treat the diffuse lesion ASAP. The flow of the branch of OM decreased from TIMI 3 to TIMI 2. Progressed intramural hematoma was favored. We used another wire with Crusade for wiring to the occluded branch and a small balloon for dilatation. The flow returned. We didn't place stent and observed the flow for 15 minutes. The TIMI 3 flow preserved and we closed the procedure. After removal of all device, protamine of 30mg was applied for partial reversal. 3 weeks later, catheterization was checked and the flow of the branch was well.
 9.mp4
9.mp4
 17.mp4
17.mp4
 23.mp4
23.mp4
 29.mp4
29.mp4
 31.mp4
31.mp4
 33.mp4
33.mp4
 echo1.mp4
echo1.mp4
 echo2.mp4
echo2.mp4
 39.mp4
39.mp4
 48.mp4
48.mp4
 51.mp4
51.mp4
 54.mp4
54.mp4
 58.mp4
58.mp4
 61.mp4
61.mp4
 62.mp4
62.mp4
 66.mp4
66.mp4


Case Summary
1. Learning Points: Early identification, Serial echocardiography, Hemodynamic monitoring
