CASE20220714_001
A challenging Case Report : Multiple bifurcation approach in patient with ACS
By
Presenter
Imad Sheiban
Authors
1
Affiliation
, Italy1
Complex PCI - Bifurcation/Left Main Diseases and Intervention
A challenging Case Report : Multiple bifurcation approach in patient with ACS
1
, Italy1
Clinical Information
Patient initials or Identifier Number
GT
Relevant Clinical History and Physical Exam
78 yrs male. Risk factors : Familiarity , Hypertension, dyslipidemiaComorbidities: COPD, mild renal Failure, previous strokeClinical History : 2015 first episode of chest pain on exertionand hypertension . Treated with beta-blockers, ACE inmhibitors and ASA. . No symptoms till 2022.April 2022: admitted to the hospital for prolonged chest pain. At Admission : BP = 145/95 mmHg, HR=68 bpm, O2 saturation 96%. Killip Class 1 .Shifted to Cath Lab for coronary angiogarphy
Relevant Test Results Prior to Catheterization
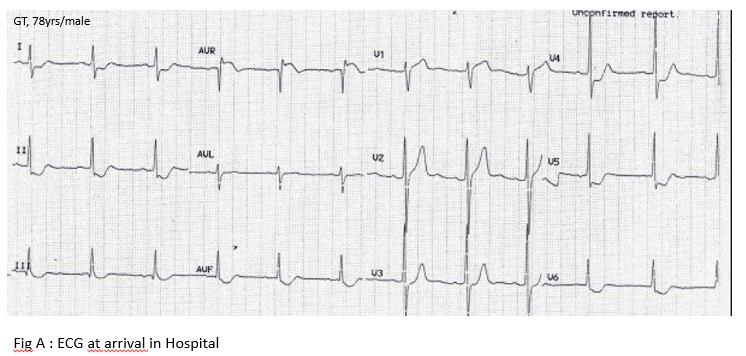
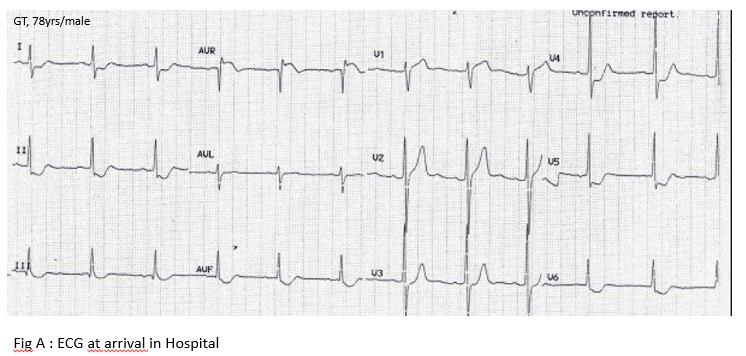
Blood Tests: Creatinie : 135 umol/l , Glucose : 5,7 mmol/l, Hb : 13,2 g/dL, RBCs : 4,6 106 /uL , WBCs : 8.5 103 /uL , Platelets : 195 103 /uL, , CRP : 7.7 ng/dlT-Troponine (1 hour) : 75 ng/L T-troponine ( 2 hours) : 174 ng/L CK-MB : 4,7 ng/mLTotal Choletserol : 5.8 mmol/lLDL cholesterol : 3.86 mmol/lHDL Cholesterol : 1,21 mmol/lTriglycerides : 2,2 mmol(l ECG : ST/T depression in nterior wall ( Fig A) ECHO : Anterior Hypokinesia- LVEF = 0.46
Relevant Catheterization Findings
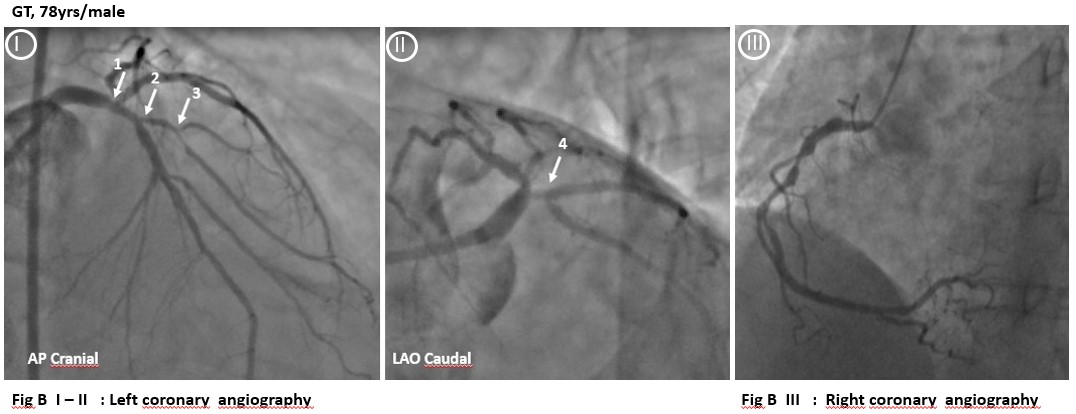
Coronary angiography : Distal Left main with 3- vessel disase Distal left main stenosis involving both LAD and LCX ostium Medina 1,1,1 confirmed on OCT LAD - 1st diagonal disease Bifurcation disease -Medina 1,1,1 - ( Large bifurcated diagonal branch with long prosximal lesion ) LCA -OM bifurcation lesion - Medina 1,0,1 -RCA : long lesion
Syntax Score = 32Syntax Score II : PCI : 39.3 - 4-yr Mortality 14,3%CABG: 53.1 - 4-yr Mortality 38.7%
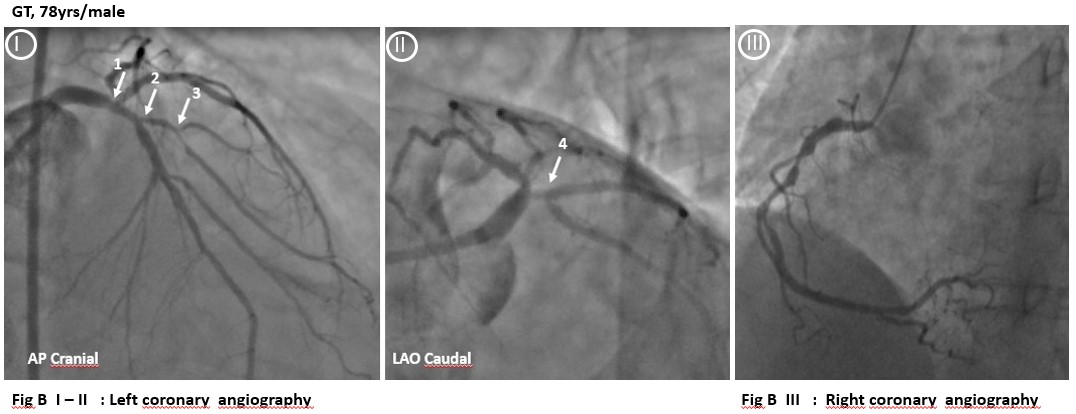
 Fig B I.avi
Fig B I.avi
 Fig B II.avi
Fig B II.avi
Syntax Score = 32Syntax Score II : PCI : 39.3 - 4-yr Mortality 14,3%CABG: 53.1 - 4-yr Mortality 38.7%
Interventional Management
Procedural Step
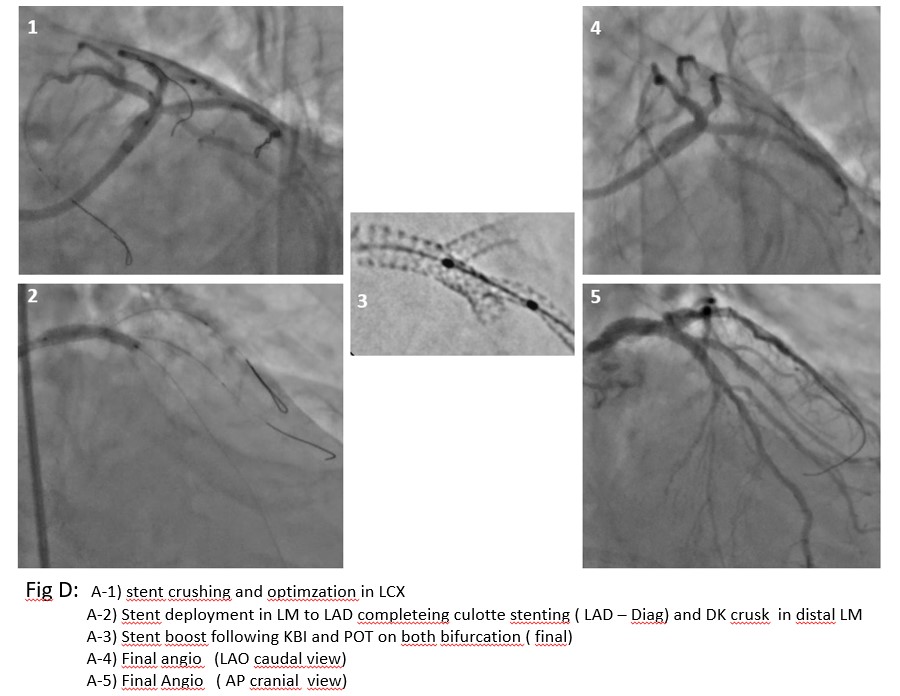
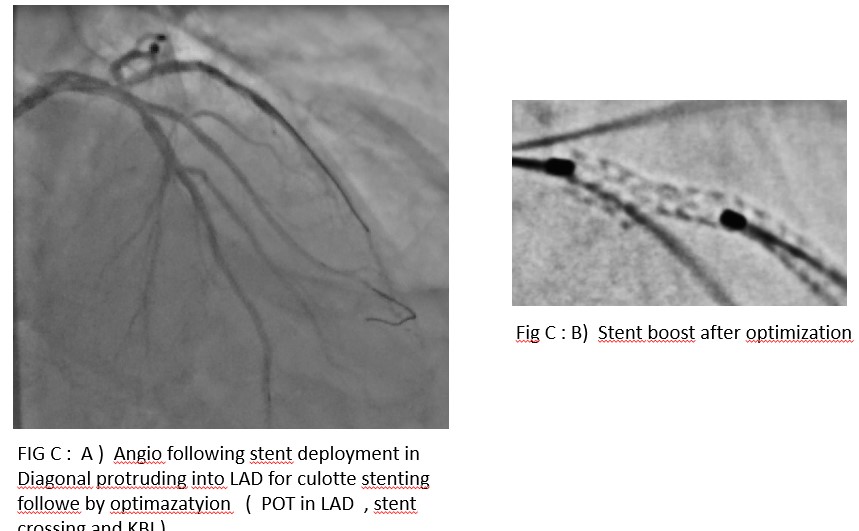
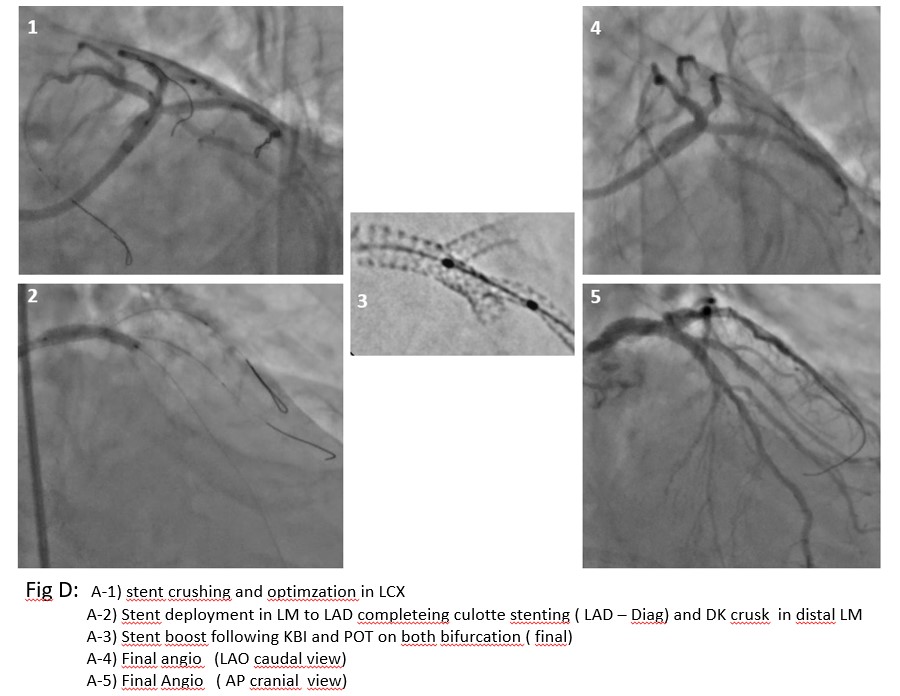
Heart Team discussion ( + patients preference ) : :PCI option Plan : Femoral access- 7F guiding catheter .- Intravascular imaging ( OCT ) to better define LM and LAD lesions and to plan accordingly the strategy OCT : significant disease in distal LM ( MLA= 4.4 mm ) diffuse diseasin prox LAD (MLA 2.9 mm ) , severe lesione at LCX ostium ( MLA = 2,1 mm) . Strategy : miniCulotte at LAD-1st Dig bifurcation and DK minicrush at distal LM both realizes with a single stent from LM to LAD. Stepwise approach : Wiring LAD and Fisrta Diagonale and LCX Predilatation in Diagonal -LAD . HP deployment of Xience stent 2.75x23mm in I diagonale protruding 2 struts ina LAD . POT In LAD - Recrossing the stent with awire to LAD - Stent strut Dilatation with 1-1 balloon. KBI ( LAD-LAD nd LAD - Diag ) and POT ( Fig C)Predilatation LCX . Xience Stent 3.0x15 mm on the wire to LCX with minimal protrusion in LM and balloon on LAD wire in crossover LM-LAD . Stent in LCX depoluyed at HP . Delivery balloon retrieved . Protruded segment of the stent in LM crushed with the balloon already on site. Recrossing proximale the crushed setnt with a wire to LCX - 1st KBI (LM-LAD-LCX) and deployment of Xience 3.5 x 23 mm from LM to LAD completing both miniculotte ( LAD- Diag) and DK cruish ( distal LM) with the same stent. POT in LM- recrossing the stent with a wire to Diag and another to LCX . KBI and POT at LAQD-Diag Bifurcation and 2nd KBI and POT in LM Bif.( Fig D)Final OCT runs : LAD to LM and LCX to LM. Final angio
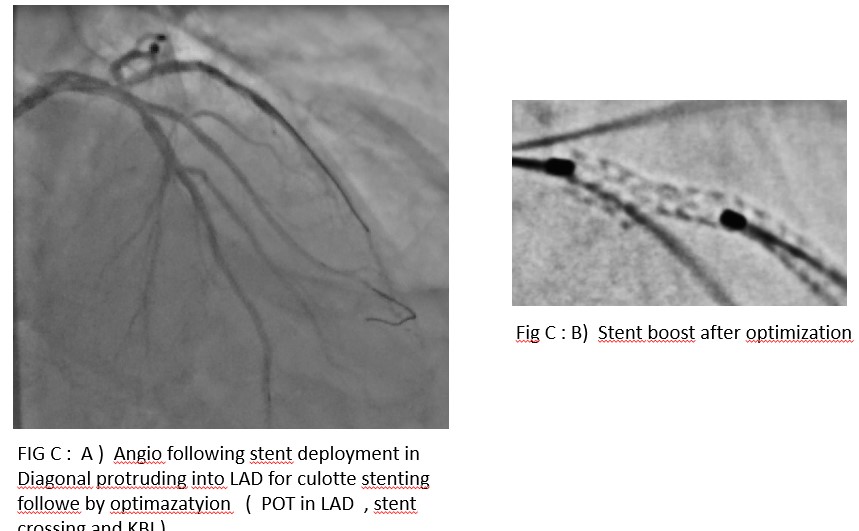
 GT following Diag stenting and optimization.avi
GT following Diag stenting and optimization.avi
 GT- AVI Fig D 5.avi
GT- AVI Fig D 5.avi
 GT AVi Fig D4.avi
GT AVi Fig D4.avi
Case Summary
My take home message : Complex stenting in bifurcation lesion and particularly in distal Lm is challenging .Intravascular imaging is essential to appropriately define distal LM disease and to plan the most appropriate approach Operator experience in BL interventions and stepwise approach can help in making complex stenting simple Intravascular imaging based final optimization is always recommended
